
by Stemedix | Oct 10, 2022 | Alzheimer’s Disease, Stem Cell Therapy
Alzheimer’s disease is one of the most prevalent neurological conditions in the world, affecting more than 5.8 million people in the United States alone. While millions of people suffer from the condition, not everyone understands how Alzheimer’s really affects the brain. So how does Alzheimer’s affect the brain? Keep reading to find out!
How Alzheimer’s Impacts Your Brain
Alzheimer’s is a progressive neurological disease that results in damage to the brain. Alzheimer’s attacks the regions of the brain that are responsible for memory and language. This leads to severe memory loss and other cognitive symptoms.
The exact cause of Alzheimer’s is still largely unknown, but it has been linked to the buildup of plaque within the brain. It is also thought to be genetic in some cases, affecting multiple people from the same family.
Symptoms of Alzheimer’s
Treating Alzheimer’s relies heavily on an early diagnosis. In order to detect the disease as early as possible, you should be on the lookout for signs and symptoms that could indicate changes within the brain. The following are some of the most common signs of Alzheimer’s disease:
- Difficulty completing familiar tasks
- Unable to recall everyday information
- Getting lost in familiar locations
- Frequently misplacing things
- Mood swings and extreme behavioral changes
- Uncharacteristic decision-making
- Difficulty with finances
- Sudden poor hygiene or unkept home
While these symptoms can sometimes be attributed to mental health disorders like depression, they are often indicators of Alzheimer’s disease, particularly in older individuals. When you notice these signs in yourself or a loved one, being evaluated by a neurologist as soon as possible is vital for successful treatment.
Treating Alzheimer’s Disease
The way Alzheimer’s disease is treated has evolved in recent years. In the past, there were very few options in terms of slowing the progression of Alzheimer’s. Patients and their loved ones relied on behavioral intervention and other therapeutic approaches to cope with the symptoms of the disease.
Thanks to recent research, now there may be alternative options to help slow down the progression of Alzheimer’s and reduce the severity of symptoms.
One innovative approach involves regenerative medicine, also known as stem cell therapy. A patient’s own stem cells could potentially be used to heal the damage that Alzheimer’s causes to certain areas of the brain. Stem cell therapy also provides regenerative properties that could produce new neurons, replacing any damaged cells within the brain.
Research on stem cells as a treatment for Alzheimer’s is ongoing, but studies have shown that the approach is most effective when a patient is in the earlier stages of the disease. To learn more about ” How does Alzheimer’s affect the brain? ” and the options available at Stemedix, contact a care coordinator today!

by Stemedix | Oct 3, 2022 | Chronic Fatigue Syndrome, Stem Cell Therapy
Chronic fatigue syndrome (CFS) is a collection of symptoms that make work, relationships, and personal achievement more difficult. Patients with CFS cannot pinpoint other underlying disorders or diseases as the cause of their symptoms.
If chronic fatigue syndrome is taking over your life, there is a promising potential solution: regenerative medicine therapy.
How Regenerative Medicine May Help
Regenerative medicine, also known as stem cell therapy, works by harnessing your body’s ability to regenerate healthy cells.
When you suffer from a complex disorder like chronic fatigue syndrome, your healthy cells and tissues are constantly under attack. Stem cell therapy may be able to rebuild damaged cells so you can experience the relief you have been seeking.
Pain Management
Common symptoms of CFS include muscle pain and weakness. Sufferers of CFS also report frequent headaches that can be debilitating.
Stem cell treatments have the potential to provide long-term pain relief using your body’s natural regenerative processes. If you are looking for an alternative method of pain relief, stem cell therapy might be for you.
Immune System Regulation
Chronic fatigue syndrome is believed to be a type of autoimmune disorder. This means that your immune system incorrectly identifies your own cells and tissues as threats.
Stem cell therapy can help regulate patients’ immune systems in some cases. This would prevent your immune system from continuing the cycle of draining symptoms you experience with CFS.
Energy Boost
A key sign of chronic fatigue syndrome is constant exhaustion. No matter how much sleep, you probably feel like you had no rest at all.
Stem cell therapy has the potential to boost your energy levels by repairing and rebuilding essential cells and tissues. Your body has been under attack for a long time, but stem cell therapy may be able to break the cycle.
The Power of Stem Cells in CFS Therapies
Since stem cells can develop into almost any type of specialized cell in your body, they can be powerful tools for rejuvenating your health. Your body follows certain processes to repair and regenerate cells and tissues. Stem cells kick-start these processes and provide more resources for repair.
Managing CFS is about relieving symptoms. If your daily life is affected by chronic fatigue syndrome, stem cell therapy might be worth exploring to potentially improve how you feel. This experimental therapy is natural and has been studied to be safe and provide the potential for symptom relief. To learn more about the options available at Stemedix, contact us today!

by admin | Oct 1, 2022 | Stem Cell Therapy, Exosomes, Extracellular Vesicles, Mesenchymal Stem Cells, Stem Cell Research
The number of people experiencing autoimmune diseases (ADs) continues to increase worldwide. Currently, it’s estimated that between 2 and 5% of the global population is afflicted with the most severe forms of these diseases, including type 1 diabetes (T1DM), systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA).
An autoimmune disease can occur nearly anywhere in the body and is the result of the immune system mistakenly attacking your body instead of protecting it. While the reason this occurs is not yet fully understood, there are over 100 different types of autoimmune diseases classified into two types: organ-specific (T1DM) and multiple system-involved conditions (SLE and RA).
In addition to T1DM, SLE, and RA, other common autoimmune conditions include Crohn’s disease, ulcerative colitis, psoriasis, inflammatory bowel disease (IBS), and multiple sclerosis (MS).
In addition to not fully understanding why these conditions occur, conventional treatments (mainly in the form of immunosuppressants) alleviate associated symptoms but do not provide lasting or effective therapy for preventing or curing these diseases.
In recent years, mesenchymal stem cells (MSCs) and MSC-derived extracellular vesicles (MSC-EV) have demonstrated immunosuppressive and regenerative effects, and are now being investigated as promising new therapies for the treatment of ADs. In this review, Martinez-Arroyo et al. provide a complete analysis of current MSC and MSC-EV efforts in regard to some of the most severe ADs (T1DM, RA, and SLE) as a way to demonstrate progress in the discovery and application of new stem cell therapies for the treatment of ADs.
Initial research by the International Society of Cellular Therapy in 2006 established that MSCs are able to exert a range of biological functions, with the most well-known being immunosuppressive and regenerative effects, suggesting that MSCs-based therapies for the treatment of ADs is possible. Additional research has also demonstrated MSCs role in regenerative medicine to be safe and effective in treating a wide variety of diseases and injuries.
Further study has demonstrated that MSCs influence immune cell proliferation, differentiation, and function. While this is promising, research also suggested that the microenvironment influences the induction, increase, and maintenance of MSCs immunoregulatory role.
Considering this, the authors of this review suggest that blocking immune cell reprogramming while maintaining MSC roles in the immune microenvironment would provide new insights into identifying strategies for the biological treatment of ADs.
Current research and findings also support the use of MSC for the regeneration of tissue. This same research has also raised concerns related to cell survival, genetic instability, loss of function, and immune-mediated rejection. Because of this, Martinez-Arroyo et al. call for further study to better understand the biology, biomaterials, and tissue engineering used during MSC therapy.
The authors conclude this review by pointing out that there has been a revolutionary change in perspective in the field of MSC-based therapies for the treatment of AD primarily stemming from the use of MSC-EVs as potential therapeutic options.
Additionally, when comparing the use of MSCs to MSC-EVs, the authors highlight several advantages demonstrated by MSC-EVs. These advantages include providing stability and safety, avoiding tumorigenesis, genetic mutability, and immunogenicity when compared to MSCs, and allowing for several modifications to their surface and cargo – all enhancing their potential as viable treatment options for ADs.
While MSC-EVs demonstrate tremendous potential, the authors call attention to the fact that the use of MSC-EVs is still in the initial research and development phases and faces major obstacles and limitations in a number of areas, including overcoming the optimization of methods for MSC-EV characterization, high-scale production, and purification and improving MSC-EV targeting.
Considering these limitations, Martinez-Arroyo calls for further research with animal models and clinical assays as a way to test the safety and efficiency of using MSC-EVS as cell-free therapy for ADs.
Source: “Mesenchymal Stem Cell-Derived Extracellular Vesicles as Non ….” https://www.mdpi.com/1999-4923/14/4/733/htm.

by Stemedix | Sep 19, 2022 | Stem Cell Therapy
Sciatica pain radiates from the lower spine down the back of your leg. Pain from the sciatic nerve can vary from sharp and jolting to a mild ache. Some sufferers find it worsens when they perform small actions, like coughing or sneezing. In addition to pain, sciatica can cause numbness, muscle weakness, or tingling. While surgery offers a treatment option for some with sciatica, results can be inconsistent and often include a long recovery. Here we will discuss the nonsurgical therapy options for sciatica pain.
What Is Sciatica?
Sciatica refers to pain stemming from the sciatic nerve. Beginning in the lower spine, the sciatic nerve splits and extends down both legs, all the way to the feet, making it the largest nerve in the body.
Often sciatica results from a problem in the lumbar spine, such as a herniated or bulging disc that compresses the nerve and creates pain that travels throughout one side of the body.
Nonsurgical Therapy Options for Sciatica
Once sciatica is diagnosed correctly, patients can explore treatment options. Frequently, patients can find relief without surgery. Some of the most effective non-surgical treatments include:
Physical Therapy
Often, physical therapy is the first treatment a physician recommends for those suffering from sciatica. The exercises and movements used in physical therapy strengthen and restore the range of motion to the core, buttocks, pelvis, and legs.
Physical therapy focuses on reducing nerve and muscle spasms, improving mobility, fostering the spine’s healing, and restoring proper function to the lumbar spine and sacroiliac joint.
Medications
Over-the-counter or prescription anti-inflammatory medications, such as acetaminophen, ibuprofen, and naproxen, and prescription medications, such as muscle relaxants, may offer patients temporary relief from their sciatica pain.
In addition, patients can use some topical medications in conjunction with oral medications, including:
- Menthol
- Capsaicin
- Camphor
- Methyl salicylate
Topical treatments often provide pain relief with fewer side effects than oral medications.
Steroid and Nerve Blocking Injections
Steroid and nerve blocking injections are common and effective treatments to reduce pain and increase functionality temporarily.
A physician administers steroid injections and a local anesthetic into the space surrounding the nerve roots and spinal cord. Nerve blocking injections use live X-ray guidance to target the area where the nerve is compressed and turn off pain signals traveling to the brain.
Nerve blocks can be administered independently or in conjunction with steroid injections.
Regenerative Medicine
Recently, regenerative medicine which can include stem cell or platelet-rich plasma (PRP) injections have provided an promising therapy option for sciatica. Both stem cells and PRP injections use the body’s natural healing properties to repair damaged cells, restore function, and reduce pain.
These options may offer relief by reducing inflammation and accelerating the healing process. As a result, they are emerging as a preferred alternative to treatments like steroid injections, which can result in long-term side effects that include cartilage and nerve damage. These side effects can exacerbate sciatica symptoms. If you would like to learn more about the Nonsurgical therapy options for sciatica, contact Stemedix today!

by Stemedix | Sep 12, 2022 | Stem Cell Therapy, Stem Cell Research, Traumatic Brain Injury
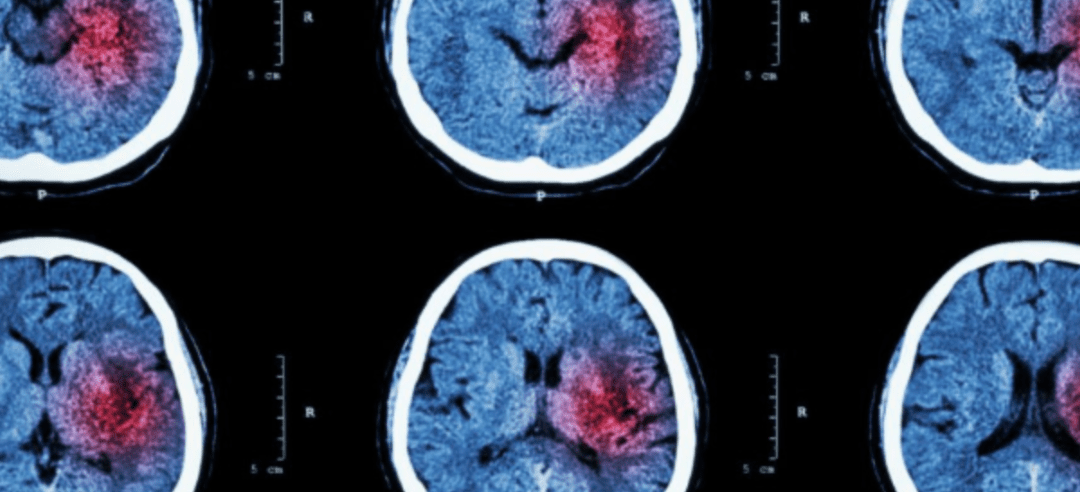
Every year, approximately 350,000 Americans experience severe and moderate traumatic brain injuries (TBI) that can result in long-term disabilities. Unfortunately, there are no effective treatments to improve the structural repair and recovery of function in patients who suffer from a TBI. Regenerative medicine methodologies, and stem cells, in particular, offer the most promising options for repairing damage and restoring performance for patients with long-term effects from a TBI. Here we talk about how stem cells help brain injury and the science behind it.
What Are Stem Cells?
Stem cells are special, due to their ability to become new types of cells. The entire human body originated as a cluster of stem cells. Stem cells are the only cells in the body that can divide to create specialized cells, such as brain or blood cells.
Since many specialized cells, like neurons, cannot divide to create new cells, stem cells’ unique ability to differentiate into the needed cells surrounding them allows breakthrough alternative medicine options in patients who previously had no opportunities for recovery.
What Is Stem Cell Therapy?
A physician extracts stem cells from a patient in a stem cell therapy treatment. Those cells often come from the patient’s bone marrow or fat tissue. The doctor then readministers the cells into the targeted areas.
The stem cells begin dividing to create the cells needed to repair the damage and replace dead cells. This process allows stem cells to help manage the root cause of pain, condition, and injury, instead of the traditional approach of managing and masking symptoms.
How Can Stem Cell Therapy Help Brain Injuries?
While neurons cannot divide to create new cells, adult neural stem cells can divide and should have the functionality to differentiate into neurons. In addition, the presence of these cells implies that the brain has some ability to repair itself in response to injuries or diseases affecting the central nervous system.
In the absence of the brain activating this response on its own, scientists are now researching how neural stem cells can help potentially repair a TBI through cell transplantation.
In one study, neural stem cells (NSCs) were transplanted into a damaged area of the subject’s brain and differentiated into region-specific functional cells.
While few studies using humans have reached their final stages, early reports reveal that extracted NSCs may survive for weeks upon injection into an injured portion of the central nervous system. This promising news ensures that stem cells have the time to restore damaged cells and rebuild function after an injury.
While the need for further research and results is clear, early findings offer hope that stem cells may become a widely available option to treat brain injuries. If you would like to learn more about the treatment options available at Stemedix, contact us today! We provide stem cells that help brain injury.

by Stemedix | Sep 5, 2022 | Parkinson's Disease, Stem Cell Therapy
Treating the neurodegenerative disorder Parkinson’s disease can be incredibly challenging. Since the condition’s progression varies widely, there is no standard treatment. Ideally, patients work with their healthcare provider to create a treatment plan tailored to their symptoms. Here we will discuss the current treatments for Parkinson’s Disease.
Most treatment plans include a multipronged approach, combining exercise, therapies, and medications to manage symptoms and slow the condition’s progression.
Exercises for Parkinson’s Disease
Exercise is critical to maintaining balance, mobility, and strength for those with Parkinson’s. When using physical activity to manage Parkinson’s symptoms, patients should combine aerobic, strength, balance, agility, and flexibility exercises.
Many activities incorporate these elements, such as yoga, biking, running, dance, and Pilates.
Therapies for Treating Parkinson’s Disease
Depending on the symptoms a patient experiences, several therapies can assist with mobility, speech, and function.
Physical Therapy
Many Parkinson’s patients are prescribed physical therapy to remain independent. These therapies can retrain the muscles and slow the progression of hypokinesia, or smaller movements that develop as the disease progresses.
Additionally, physical therapy can aid balance, flexibility, strength, and coordination.
Occupational Therapy
Occupational therapy allows those with Parkinson’s to remain active and find new ways to complete tasks that become more difficult as the condition progresses. Patients also learn to use new equipment to stay independent and add ease to movement.
Speech Therapy
Many patients with Parkinson’s experience speech problems such as low speech volume, hoarse or breathy speaking, or lack of pitch. Speech therapy can help with speaking mechanics, using assistive devices, and swallowing concerns.
Medications for Parkinson’s Disease
Currently, the most common medication for managing the symptoms of Parkinson’s disease is a drug called levodopa. The brain converts levodopa to dopamine, helping replace the neurotransmitter’s loss.
Since levodopa can cause nausea, the medication is almost always administered with a companion drug, carbidopa, which manages stomach upset and nausea symptoms.
Unfortunately, levodopa’s absorption is inconsistent because it takes a long path from the small intestine through the blood to the brain. The inconsistency can lead to a rise and fall in the brain’s dopamine levels.
Additionally, the treatment becomes less effective over time, as the cells that convert levodopa to dopamine continue to decline. There are several other medications aimed at reducing Parkinson’s symptoms. However, they all have some limitations.
Surgical Options
Surgical treatments for Parkinson’s disease include deep brain stimulation (DBS) and Duopa.
Deep Brain Stimulation
DBS aims to reduce patients’ movement-related symptoms. In this procedure, a surgeon implants electrodes into the brain. These electrodes deliver electrical stimulation into targeted areas that control movement.
Many patients experience a reduction in symptoms after DBS surgery. However, the amount of reduction varies, and most patients remain on their medications, though in smaller doses.
Duopa
Duopa allows carbidopa-levodopa medication to be administered directly into the intestine via a gel. This methodology improves absorption and reduces the fluctuation of dopamine levels.
Patients require surgery to place a tube in the intestine. Then, a pump delivers Duopa directly to the intestine via the tube.
New Alternative Therapy
Researchers are seeing promising results in investigating regenerative medicine, also known as stem cell therapy, for managing Parkinson’s disease. Early studies offer hope that stem cells will provide a more comprehensive option to manage Parkinson’s symptoms. If you would like to learn more about the treatment options available at Stemedix for Parkinson’s Disease, contact a care coordinator today!





 St. Petersburg, Florida
St. Petersburg, Florida
