
by admin | Sep 27, 2023 | Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Wharton's Jelly
Mesenchymal stem/stromal cells (MSCs) continue to be viewed as a source of cell therapy applications due to their immunomodulatory and anti-inflammatory effects and because of their ability to stimulate angiogenesis. In MSCs, these benefits are mainly attributed to the secretion of factors.
Despite MSCs’ known and favorable proliferation levels, multipotency, and immune response regulation, there are other important variables that should be considered when developing cell therapy applications, including the source of MSCs.
Considering that MSCs collected from different tissues can form heterogeneous cellular populations and manifest tissue-specific functional differences, the source of MSCs should be of primary consideration when developing new therapeutic approaches.
In this review, Paladino et al. present a review of recent research related to the therapeutic application of Wharton’s jelly MSC (WJ-MSC) harvested from umbilical cords and how these cells affect immune responses in comparison with other sources of MSCs.
Bone marrow-derived stem cells BM-MSCs have long been considered the favored source of MSCs and are the most used source of MSCs in clinical research. However, BM-MSCs have a history of showing mixed results and are not always recommended for use due to the invasive and painful process used to obtain the MSCs.
While other alternative sources, including adipose tissue, dental pulp, and menstrual blood, are available, WJ-MSCs are considered an easily accessible source of MSCs that are comparable to BM-MSC and have suffered less environmental interference and demonstrate higher proliferative capacity than other sources.
One of the most promising benefits associated with MSC therapy is the potential to treat inflammatory or autoimmune diseases, including systemic lupus erythematosus, type 1 diabetes, and multiple sclerosis.
Studies using WJ-MSC in this capacity have shown their robust immunomodulatory potential. Specifically, the authors of this review reference a number of studies using various sources of MSCs, including WJ-MSCs that demonstrate immunomodulatory potential similar to other MSC sources. Studies also demonstrate that WJ-MSC is a better suppressor of specific inflammatory factors, including mixed lymphocyte reaction, and possesses higher levels of IL-17A (a key mediator in the treatment of graft-versus-host disease) than MSCs collected from other sources.
Paladino et al. conclude that the available literature indicates that WJ-MSCs possess immunological features comparable to MSCs from other sources, including bone marrow-derived MSCs. The authors also call for further study to identify the best therapeutic indications for WJ-MSCs as a substitute for other sources of MSC, including BM-MSC.
Source: “The Immunomodulatory Potential of Wharton’s Jelly Mesenchymal ….” 11 Jun. 2019, https://www.hindawi.com/journals/sci/2019/3548917/.

by admin | Aug 9, 2023 | Mesenchymal Stem Cells, Stem Cell Therapy, Wharton's Jelly
Human umbilical cord Wharton’s Jelly derived mesenchymal stem cells (WJ-MSCs) are reported as the most potent cell source of MSCs, however, they remain understudied in comparison to other autologous sources of MSCs.
Mehling et al.’s study aimed to evaluate the safety of WJ-MSC therapy for a range of conditions and administration routines, including intravenous, intrathecal, and intra-articular delivery.
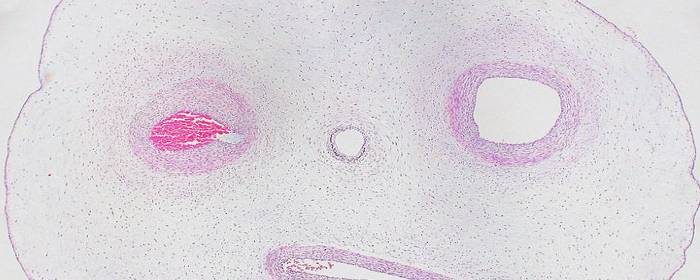
Wharton’s jelly (WJ) is the mucoid connective tissue that surrounds the vessels in the human umbilical cord and provides protection from compression and torsion in response to fetal movement.
According to this study, the use of WJ-MSCs has many advantages over autologous MSCs, including circumventing the pain and healing process of invasive stem cell harvesting from a patient. Additionally, WJ-MSCs offer the highest level of potency for therapeutic benefit and exhibit increased proliferation ability and anti-inflammatory effects.
Additionally, WJ-MSCs have been demonstrated to be safe and effective for many conditions. WJ-MSCs also do not cause or contribute to infusion-related toxicity, treatment-related adverse events, or ectopic tissue formation, even when administered at high dosages.
In this study, Mehling et al. confirm the safety of human allogeneic WJ-MSCs delivered at high doses and through multiple delivery routes (including intravenous (IV), intrathecal (IT), and Intraarticular (IA)).
Specifically, as part of this study, 22 subjects were evaluated for adverse events (AEs) for a period of 6 months following treatments with WJ-MSCs for a range of conditions, including neurological and osteoarthritic indications.
At the conclusion of the 6-month period of evaluation, the study reported an AE rate of 9.3% (3 subjects from the 32 doses administered in this study). The reported AEs consisted of chills and headaches, both transient and mild, and resolving without concern. While both of these AEs (headache and chills) are relatively common reactions to cell administration, 1 of the 3 AEs was deemed related to the administration procedure.
Additionally, blood profiling of 75 markers for health and disease in the subjects of this study demonstrated that WJ-MSC treatment poses no hematological safety concerns.
Considering the minimal occurrences of AEs observed following WJ-MSC therapy administered during this study, the authors support the use of WJ-MSC therapy for various indications in future clinical studies.
Source: “Safety study of cultured human Wharton’s Jelly mesenchymal stem ….” https://www.cellr4.org/wp-content/uploads/sites/2/2022/10/e3332.pdf.

by admin | Jan 5, 2023 | Mesenchymal Stem Cells, Diabetes, Regenerative Medicine, Stem Cell Research, Stem Cell Therapy, Umbilical Stem Cell, Wharton's Jelly
Mesenchymal stem cells (MSCs) are multipotent fibroblast-like cells found throughout the body and have been found to have self-renewing and multilinear therapeutic potential by providing new cells for tissue repair by replacing damaged cells.
Thought to stimulate repair and control the immune response through an expression of growth factors and other cytokines, MSCs are at low risk of rejection and repair tissue damage through immunomodulation, not by their ability to differentiate.
While MSCs can be isolated from a number of tissue sources, including bone marrow, peripheral blood, adipose (fat) tissue, umbilical cord blood, and umbilical cord tissue (Wharton’s jelly). MSCs derived from the human umbilical cords (UCMSCs) have been found to have significant advantages over MSCs isolated from other sources. These advantages include higher proliferation and self-renewal capacity and multilineage differentiation capability.
Unlike many sources of MSCs, the umbilical cord is considered medical waste, making the collection of UCMSCs noninvasive and eliminating ethical concerns associated with the collection of MSCs from other sources. These UCMSCs have been developed as effective “off-the-shelf” cell therapy for a number of conditions, including autoimmune diseases, and as a treatment for a number of emergency medical conditions.
This Phase 1 clinical study, designed and conducted by Chin et al., intended to determine the safety and efficacy of intravenous allogeneic infusion of UCMSCs in healthy volunteers and to determine the effective dose at which an immunomodulatory effect is observed. The findings of this study are intended to serve as a guideline and benchmark for future CVL-100 clinical research.
Analyzing the results of this clinical study, the authors report that there was no observed complication resulting from the infusion and no significant adverse event in either dosage group in the 6 months of follow-up. These findings led Chin et al. to conclude that UCMSCs infusion was safe among healthy subjects, results that were consistent with other UCMSC treatment-based studies.
The authors also reported that UCMSCs infusion posed no significant adverse effects in patients with type 2 diabetes. Despite the relatively small sample group of this study (11 subjects), the authors reported demonstrating an initial transient proinflammatory effect followed by a significant and prolonged anti-inflammatory effect.
In addition, Chin et al. report found that high-dose (HD) CLV-1000 infusion provided a significant increase in both hemoglobin level and MCV level that falls within the normal range. Biomarker assessment results also indicated that the HD group demonstrated a significant steady increase of cytokine IL-1RA from baseline up until 6 months of posttreatment. This finding is especially important as IL-1RA is a naturally occurring antagonist to the proinflammatory cytokine 1L-1.
The authors conclude that this study clearly demonstrates a difference in immunomodulatory effect between the high-dose and low-dose treatment groups, with the HD group demonstrating a significantly greater reduction of proinflammatory cytokine TNF-α and an increased level of specific anti-inflammatory cytokines within 6 months and in relation to those in the low dose group. Considering this, Chin et al. conclude that a CLV-100 dosage of two million MSCs per kilogram of body weight represents the optimal dose level for overcoming inflammatory conditions by displaying the best improvement in all parameters tested, absence of side effects, and SAEs.
The data collected in this study also suggests that this is the first study to report a significant reduction of globulin observed over the course of the study. This is important because globulin serves an important role in immunity. Additionally, increases in serum globulins are associated with several immune-mediated diseases, including rheumatoid arthritis, chronic liver disease, diabetes mellitus, and cancer.
Considering these findings, the authors of this study conclude that high doses of allogeneic MSCs could help exert beneficial effects of repair and healing.
Source: “High Dose of Intravenous Allogeneic Umbilical Cord-Derived ….” https://www.hindawi.com/journals/sci/2020/8877003/.

by admin | Apr 1, 2022 | Stem Cell Therapy, Adipose, Mesenchymal Stem Cells, Musculoskeletal, Wharton's Jelly
Articular cartilage, found on the surface of most musculoskeletal joints, distributes and transfers forces between bones and joints, provides a smooth surface for joint mobility, and plays an important role in human mobility.
However, articular cartilage is also easily susceptible to damage, but difficult to repair itself on its own (primarily due to the fact it is mostly avascular). Over time, the inability of articular cartilage to repair itself leads to progressive joint pain, disfigurement, movement disorders, and ultimately osteoarthritis.
The CDC estimates that nearly 33 million Americans are currently affected by osteoarthritis, most often in the form of pain, stiffness, decreased mobility and range of motion, and swelling in the joints[1].
Current treatment methods, including microfracture technology, autologous or allogeneic cartilage transplantation, and autologous chondrocyte implantation (ACI) have demonstrated the ability to repair and regenerate fibrous cartilage, but not articular cartilage required for smooth, fluid, natural mobility.
To address this issue, recent research has focused on the efficacy of stem cells, and specifically mesenchymal stem cells (MSCs) found in bone marrow, adipose tissue, synovial membrane, and umbilical cord Wharton’s jelly, as potential therapeutic treatments for regeneration of articular cartilage. MSCs are particularly of interest due to their demonstrated abilities of self-renewal, multi-differentiation, and immunoregulation.
While the use of MSCs has demonstrated tremendous potential in the field of regenerative therapy, one notable drawback continues to be unstable or suboptimal results resulting from the heterogeneity of various mesenchymal stem cells.
Specifically, the stability and efficacy of MSCs appear to differ based on a number of factors, including the donor, the tissue source, and their ability for proliferation, differentiation, and immunoregulation.
For example, some of the key heterological differences highlighted in this review include the efficacy of MSCs based on donor’s age (with younger donors providing higher quality MSCs), Wharton’s Jelly MSCs showing greater prospects for application in cartilage regeneration than other MSCs, and differences within specific MSC subpopulations.
The authors of this review acknowledge the potential of MSCs in repairing arterial cartilage, but also point out that there needs to be a deeper understanding of the heterogeneity of various MSCs in order to improve the efficiency of MSC-based therapies designed to repair arterial cartilage. In addition, the authors also call for greater standardization in MSC isolation and harvesting methods among laboratories in order to provide better consistency with respect to results obtained from studies using MSCs.
Source: “Heterogeneity of mesenchymal stem cells in cartilage regeneration.” 19 Mar. 2021, https://www.nature.com/articles/s41536-021-00122-6?elqTrackId=5517bd20493b470cb34fd0e8bc1f6ef9.
[1] “Osteoarthritis (OA) | Arthritis | CDC.” https://www.cdc.gov/arthritis/basics/osteoarthritis.htm.

by admin | Nov 28, 2018 | Stem Cell Therapy, Wharton's Jelly
Perinatal stem cells have been attracting attention globally in recent years due to their potential in regenerative medicine. These stem cells come in many forms, due to the wide variety of potential sources for these cells. Perinatal stem cells, for instance, may be umbilical cord-derived hematopoietic stem cells, amniotic epithelial cells, amniotic fluid stem cells, or chorionic mesenchymal stem cells. All sources, nonetheless are considered biological waste and are therefore usually discarded after delivery of babies.
Importantly, perinatal stem cells, despite their origin, tend to share a number of characteristics that make them beneficial in treating conditions. Additionally, unlike other sources of stem cells, retrieval of perinatal stem cells is noninvasive and does not require the ethical considerations that retrieval from other sources may involve. A recent review in Regenerative Medicine has highlighted the potential benefits of perinatal stem cells in therapeutic interventions.
In addition to the relatively easy collection and preparation of perinatal stem cells, these cells tend to be easily harvested and manipulated without harming either the mother or the baby. Upon collection, these stem cells exist in high volume and have greater ability to proliferate than other stem cell types such as bone marrow stem cells. Research has also shown that these cells tend not to lead to adverse immune reactions, though the mechanisms involved in their relationship to the immune system are not well understood.
Given their relative advantages over other stem cell types, perinatal stem cells are well poised to be used in cell-based therapies targeting a wide variety of conditions. Future research will help to define the precise role these cells can play in regenerative medicine and which conditions they may be most useful for.

by admin | Oct 4, 2018 | Stem Cell Therapy, Lupus, Wharton's Jelly
Wharton’s jelly is a rather unique body fluid. It is the connective tissue found within the umbilical cord. While Wharton’s jelly is connective tissue, it more closely resembles gelatin. Historically this material was discarded as medical waste; however, Wharton’s jelly has been shown to contain a number of therapeutic substances. Among these healing substances found within Wharton’s jelly is an abundant supply of mesenchymal stem cells.
One of the most intriguing features of Wharton’s jelly is that it contains a virtually limitless supply of mesenchymal stem cells. There are about 4 million new births in the United States each year, 5 million in the European Union, and over 100 million worldwide. The potential pool of cells is staggering when you consider only a small amount of Wharton’s jelly can contain millions of stem cells. Notably, Wharton’s jelly is usually discarded after the delivery of a healthy baby. If this material could be donated instead of discarded, researchers believe they have found an abundant, renewable resource from which to draw mesenchymal stem cells.
However, the abundance of Wharton’s jelly is not the most impressive feature of the substance. The stem cells found in Wharton’s jelly are rather unique. Perhaps most importantly, the cells are immuno-privileged. This means they are not readily recognized by the immune system. Consequently, the stem cells can be taken from the umbilical cord, purified, and then injected into a patient with little risk of the patient having an immune reaction to the cells. These particular mesenchymal stem cells are also interesting because they are relatively “primitive,” which means they have some of the same properties of embryonic stem cells. However, Wharton’s jelly can be obtained without controversy, while harvesting embryonic stem cells from aborted tissue remain highly controversial.
Stem cells taken from Wharton’s jelly are already being used in some clinical studies. For example, researchers in one clinical study injected type 2 diabetes patients with Wharton’s jelly-derived mesenchymal stem cells. Within six months of treatment, 7 of 22 patients became insulin-free and 5 were able to reduce the amount of insulin they needed by more than 50%. Only one patient out of the 22 did not respond to the stem cells at all. The cells have also been tested in systemic lupus erythematosus, better known as simply lupus. Forty patients received Wharton’s jelly mesenchymal stem cells intravenously. Thirteen patients enjoyed a major clinical response while 11 enjoyed a partial clinical response of their lupus symptoms.
As more clinical studies are done on Wharton’s jelly-derived mesenchymal stem cells, we will learn what other diseases can be treated with this once-discarded substance. Early indications show a very promising future.

 St. Petersburg, Florida
St. Petersburg, Florida
