Targeting Neuroinflammation and Glial Scar Formation in Spinal Cord Injury: The Emerging Role of Mesenchymal Stem Cells
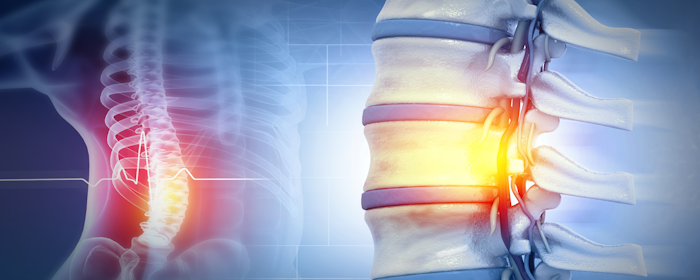
Spinal cord injury (SCI) is a devastating neurological condition that disrupts communication between the brain and body. The injury unfolds in two major phases. The primary injury occurs at the moment of trauma, such as a fracture or dislocation of the vertebrae, which directly damages neurons and axons. This mechanical disruption can immediately sever nerve…