Safety and Clinical Outcomes In Chronic Ischemic Stroke Patients After Implantation of Mesenchymal Stem Cells
According to the CDC, stroke continues to be a major cause of serious disability for adults. It is also estimated that nearly 800,000 people in the United States have a stroke each year[1]. While 80% of those experiencing a stroke survive for at least one year following the event, more than 70% will continue to experience long-term disabilities.
Stroke is divided into three distinct phases: acute, subacute, and chronic phases. The acute phase of stroke occurs within 24 hours of the actual ischemic event. The subacute phase starts at 24 hours and lasts up to 3 months. The chronic phase of stroke, by definition, starts at 3 months.
While stroke patients tend to see some response to rehabilitation efforts occurring in the chronic phase, they tend to quickly plateau, leaving many with serious chronic neurological and functional disabilities. To date, there are no approved treatments for the chronic phase of stroke.
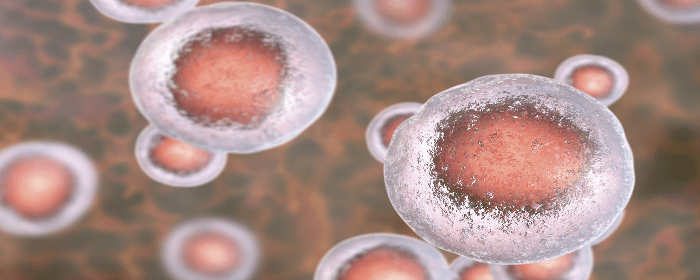
For the purposes of this study, Steinberg et al. report the two-year outcomes of their phase 1/2a study examining chronic stroke patients after implantation of mesenchymal stem cells (MSCs). This study specifically examined the outcomes of 18 patients who were at least 6 months post-stroke onset and had chronic motor deficits secondary to the nonhemorrhagic stroke.
At the 1-year point of this study, the authors reported the implantation of bone marrow-derived MSCs (BMD MSCs) was generally safe, well-tolerated, and associated with significant improvement in clinical outcomes.
There were no correlations between improvement in clinical outcomes and cell dose, baseline patient age, or baseline stroke severity. However, two years after implantation of MSCs, those enrolled in this study experienced significant improvement in motor impairment scales as indicated by a number of scores, including the ESS, NIHSS, F-M total, and FMMS scores.
Although all enrolled patients experienced at least one Treatment-Emergent Adverse Event (TEAE), with headache and nausea being the most common, 94.4% of the TEAEs were determined to be unrelated and no one withdrew from the study.
Interestingly, the authors reported that there also appears to be a significant correlation between the size of newly appearing transient lesions primarily in or adjacent to the premotor cortex – a finding that remained consistent at month 12 and month 24 of this study.
While Steinberg et al.’s reported findings are encouraging, the authors point out that the small scale and uncontrolled study design mean the findings should also be interpreted with caution.
Steinberg et al conclude that their findings associated with this completed, open-label, single-arm phase 1/2a study was consistent with the data at the 1-year point and indicated that treatment of chronic stroke with BMD MSCs after 2 years continued to be safe and was associated with sustained and significant improvements in clinical outcomes.
Given the findings of this study, the authors highlight the potential of MCSs, and specifically SB623 cells used in this study, as a potential treatment for patients with chronic ischemic stroke.
Source: “Two-year safety and clinical outcomes in chronic ischemic stroke ….” 23 Nov. 2018, https://pubmed.ncbi.nlm.nih.gov/30497166/.
[1] “Stroke | cdc.gov.” https://www.cdc.gov/stroke/index.htm.

 St. Petersburg, Florida
St. Petersburg, Florida
