
by Stemedix | Feb 26, 2024 | Parkinson's Disease, Health Awareness, Neurodegenerative Diseases, Regenerative Medicine, Stem Cell Research, Stem Cell Therapy
Parkinson’s disease causes nervous system complications. If you know someone who has struggled with this disease, you know how debilitating it can be. Parkinson’s affects mood, memory, cognition, and movement.
Fortunately, science is always advancing, and experts are learning more about Parkinson’s disease. Here are seven ways to help prevent Parkinson’s disease that are backed by scientific research.
1. Do Cardio Regularly
Cardiovascular exercise is linked to many other health benefits, but one of the most notable is reduced risk of Parkinson’s disease. Aerobic exercise, even in mild forms like walking or jogging, boosts your brain health. This improves and protects your memory, concentration, mood, and cognitive abilities as you age.
Cardio has an anti-inflammatory effect on your entire body. This is significant because researchers believe that Parkinson’s is the result of excess inflammation, among other factors. By getting a moderate to high amount of aerobic exercise each week, you can help protect yourself from developing this debilitating disease.
2. Relieve Stress in Healthy Ways
Psychological stress can be just as harmful as physical stress. Between the demands of work, family life, social circles, and hobbies, many modern Americans are more stressed than ever before.
It’s essential to reduce stress to stay healthy throughout your lifetime. Chronic high stress levels can contribute to whole-body inflammation, which is a serious risk factor for Parkinson’s disease.
Stress also reduces the volume of brain matter in areas that control memory, cognition, and movement, which are all negatively affected by Parkinson’s disease. By regularly combating stress, you can protect your brain and reduce your chances of developing this problematic condition.
Some healthy forms of stress relief include:
- Exercise
- Journaling
- Meditation
- Yoga
- Self-care days
- Getting at least eight hours of sleep at night
- Spending time outdoors
- Engaging in hobbies
These activities help you stay well-adjusted and free of stress, which weighs down your mental and physical health over time. Consider making changes in your life that cut out large sources of stress whenever possible.
3. Fill Your Plate with Veggies
Most people know that vegetables are extremely healthy. If you struggle to get your daily servings of veggies in, this information might make you reconsider your habits.
Vegetables naturally contain antioxidants, which are anti-inflammatory compounds that protect against aging and tissue damage. Filling your plate with vegetables increases your intake of antioxidants, vitamins, and minerals. All of these micronutrients contribute to better brain health and anti-aging.
When it comes to Parkinson’s prevention, this is one of the most effective steps you can take. If taste is an issue, consider adding more flavors to your meals to offset the taste of vegetables. You can also add seasoning and heart-healthy oils to make vegetables taste better.
4. Avoid Pesticides and Other Harsh Chemicals
Modern agriculture has changed a lot as humanity has progressed past the hunter-gatherer days. This means that crop growers are using more chemical pesticides than ever before. The long-term effects of these chemicals on human health are overwhelmingly negative.
Some studies have linked higher rates of Parkinson’s disease with high exposure to pesticides in farmers. The harsh chemicals used in large-scale agriculture are designed to keep bugs away from crops, but they can harm your brain health in the process.
To avoid this problem, shop organic and local whenever possible. Be mindful that many organic products can still contain certain pesticides. It’s best to shop at your local farmer’s markets and small grocery stores rather than chains.
These steps will help you access high-quality produce without exposing yourself to harsh, damaging chemicals.
5. Increase Your Vitamin D Intake
Vitamin D is incredibly important for immunity, mood, bone health, and brain health. Research has shown strong connections between Parkinson’s disease and low vitamin D levels. Now more than ever, getting enough vitamin D in your diet is essential.
You get some vitamin D from sunlight. The sun’s rays boost the amount of vitamin D in your bloodstream through chemical changes.
However, too much sun exposure is linked to skin cancer and other serious health problems. You should always wear sunscreen while spending extended amounts of time outdoors, and this can reduce the amount of vitamin D you get from the sun.
You should aim to get most of your vitamin D from your diet and supplements. Healthy sources of animal fat naturally contain lots of vitamin D. Opt for meats and dairy products that have “grass-fed” or “free-range” on the labels. These animals and their products are healthier and richer in vitamin D than factory-farmed animals.
If you struggle to get enough vitamin D in your diet, work with your doctor to find an appropriate supplement. Always consult a medical professional before starting a new medication or supplement.
6. Get Plenty of Sleep
Sleep is the most restorative and reparative process your body undergoes. Without enough sleep, your brain health is sure to suffer. Your memory, cognition, mood, and physical performance all rely on an adequate amount of sleep.
Parkinson’s disease is a neurodegenerative disorder, so it makes sense that chronic lack of sleep can raise your chances of developing it.
Healthy adults should get seven to nine hours of sleep every night. Your sleep needs may be slightly different from the recommended range. It’s important to pay attention to how you feel when you wake up.
If you wake up groggy, tired, and sluggish even after eight hours of sleep, chances are you need more. On the other hand, some people can thrive on seven to eight hours of sleep with no problems.
Sleep will protect your brain health and fight inflammation that can lead to Parkinson’s disease. Make getting plenty of shut-eye a strong priority in your life — your brain will thank you later.
7. Drink Coffee or Green Tea
Caffeine seems to have a protective effect against developing Parkinson’s disease. It’s important to get high-quality sources of caffeine. Otherwise, you may notice sleep disturbances and cardiovascular side effects. Avoid sugary, caffeinated beverages like energy drinks and soda.
Green tea and coffee both have antioxidants, which reduce inflammation and promote better brain health. You don’t have to give up your daily fix to fight Parkinson’s — in fact, it may help!
Know the Facts About Parkinson’s Disease
Stay updated on the latest information about Parkinson’s disease to reduce your risk of developing it. If you or a loved one are already struggling with Parkinson’s, therapeutic treatments like stem cell therapy may help. Ultimately, knowledge is power when it comes to fighting neurodegenerative diseases.

by Stemedix | Feb 13, 2023 | Neurodegenerative Diseases, Regenerative Medicine
While all injuries should be treated and properly resolved, there are certain injuries that can have more serious prognoses than others. Neurologic injuries are one of the more significant types of injuries someone can sustain. Injuries to the brain or spinal cord can result in various debilitating symptoms. Here we will learn more about Regenerative Medicine for Neurologic Injury.
In the past, a neurologic injury came with a dire prognosis. There were few treatment options, and many patients were left with symptoms like an inability to speak or paralysis.
Fortunately, advancements in medicine have led to an array of new treatment approaches to neurologic injuries. One way to address these types of injuries is through regenerative medicine. Learn more about how regenerative medicine can treat neurologic injuries below.
What is Regenerative Medicine?
Regenerative medicine, also known as stem cell therapy, involves stem cells that are the undifferentiated cells of a multicellular organism. These cells have the capability to produce and regenerate new cells of the same type. For this reason, stem cells can be potentially beneficial when managing numerous conditions.
Stem cells have the properties to help repair damaged cells or replace them with new, healthy ones. This has made stem cell therapy a potential approach when managing neurologic injuries.
Treating Neurologic Injury with Stem Cells
Recent studies have shown that mesenchymal stem cells can be used to manage injuries to the brain and spine. One of these studies was discussed at length at the 2022 American Academy of Neurology Annual Meeting.
A study by STEMTRA examined the efficacy of stem cells when treating patients with a TBI, or traumatic brain injury. Traumatic brain injuries occur when there is severe damage to brain tissue, resulting in the death of the tissue.
This scenario can lead to a number of symptoms, including the following:
- Loss of bowel or bladder control
- Loss of fine motor skills
- Difficulty speaking
- Impaired gait
- Paralysis
The study found that ongoing stem cell therapy helped a portion of these patients improve motor function and return to normal functional capabilities. Dexterity, gait speed, and even sensory reactions were improved with this stem cell treatment.
While studies are ongoing, stem cells are more often regarded as a potential treatment option for neurologic injuries. There is still research to be done to confirm how effective this type of regenerative medicine is for patients with grave injuries like TBI.
If you are interested in learning more about Regenerative Medicine for Neurologic Injury, you can inquire with a neurologist or regenerative medicine specialist at Stemedix for more information.

by Stemedix | Jun 13, 2022 | Neurodegenerative Diseases, Stem Cell Therapy
Regenerative medicine, also known as stem cell therapy, offers a new range of treatment options for patients suffering from neurological disorders. Here we will discuss Stem Cell Therapy for Neurological Disorders.
Neurological conditions often rely on symptom management through medication. However, stem cell therapy has begun to emerge as a new alternative management option for neurological conditions.
How Does Stem Cell Therapy Work?
Stem cells are the only cells in the human body that can differentiate into specialized cells. Stem cells lie dormant throughout the body in bone marrow, fat tissues, and various organs until they’re needed to regenerate lost or damaged tissue.
When stem cells regenerate, they undergo a process called asymmetrical division. In this process, one cell becomes a perfect replica of the stem cell, and the other cell becomes a specialized cell. Stem cells also reproduce rapidly, so they react quickly when called to action.
The new cells work to repair or replace damaged cells, heal wounds, and restore function lost through dead or damaged cells.
What Neurological Disorders Benefit from Stem Cell Therapy?
As regenerative medicine research continues to grow, studies exploring the effects of stem cell therapy on neurological disorders have shown positive results in helping to manage many conditions such as:
Cerebral Palsy
Cerebral palsy is a condition that develops before, during, or shortly after birth due to damage to the brain. Symptoms of cerebral palsy in children include poor coordination and underdeveloped reflexes.
In studies, stem cell therapy shows the potential to replace damaged or nonfunctional brain cells in cerebral palsy patients, provide support to the neurons, and reduce scarring in the brain.
Multiple Sclerosis (MS)
Multiple sclerosis is an autoimmune disease in which the immune system attacks the central nervous system and damages the nerve fibers. The damage to the nervous system interrupts the communication between the brain and the rest of the body, causing symptoms like pain, weakness, and vision loss.
Trials exploring stem cell therapy in treating MS resulted in most patients not experiencing a relapse in MS symptoms or brain lesions for five years after their treatment.
Parkinson’s Disease
Parkinson’s disease is a neurodegenerative condition in which the loss of neurons in an area of the brain stem reduces dopamine production. As a result, patients with Parkinson’s disease can experience problems with movement, muscle control, gait, and balance.
In early studies, stem cell therapies worked to replace the lost neurons, and patients saw a reduction in muscle rigidity and tremors.
While there’s plenty of work needed to understand the most effective methodology and course of treatment, early research on using regenerative medicine to treat neurological disorders points to promising results. If you would like to learn more about stem cell therapy for Neurological disorders, contact a care coordinator today at Stemedix!

by admin | Mar 25, 2022 | Mesenchymal Stem Cells, Neurodegenerative Diseases, Stem Cell Research, Stem Cell Therapy
Neurodegenerative conditions such as Alzheimer’s disease (AD), Parkinson’s disease (PD), and amyotrophic lateral sclerosis (ALS) occur when neuron populations begin to diminish. There is currently no cure for these types of diseases, though clinical trials to explore various treatment options are ongoing. In particular, regenerative medicine, also known as stem cell therapy, is being heavily researched and has shown remarkable progress in controlling these conditions.
Types of Stem Cells
Stem cells serve as the foundation for every tissue and organ throughout the body. They are unspecialized but have the incredible ability to differentiate into virtually any cell type, as well as the power to self-renew.
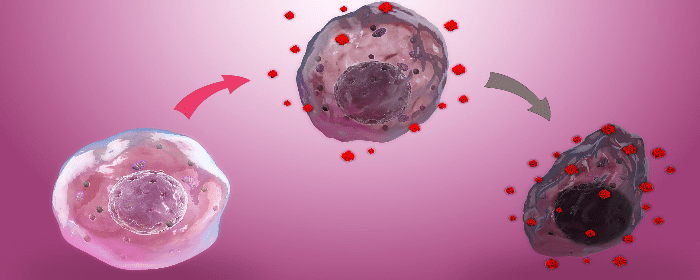
Neurodegenerative conditions are characterized by neurons that progressively lose their function and structure, and eventually die off. Because stem cells are able to differentiate into multiple cell types, researchers have begun exploring whether they could replace or repair damaged neurons to control the progression of, or potentially even reverse the damage done by, these illnesses. Existing treatment options are limited, but many researchers are optimistic about stem cells’ potential.
Not all stem cells are the same. Here are the various types, some of which show more efficacy as a treatment for neurodegenerative disease than others:
- Tissue-specific stem cells: These somewhat specialized stem cells can generate multiple organ-specific cells and are typically located in areas of the body that can self-replenish, such as the skin and blood.
- Embryonic stem cells (ESCs): Located in blastocysts, ESCs are especially promising in neurodegenerative applications. Yet, they do pose some risks, including the risk of rejection. Due to their ability to differentiate into neurons, however, they continue to be studied as a potential therapy.
- Induced Pluripotent Stem Cells (iPSCs): iPSCs are artificially derived from adult cells and programmed back to pluripotency, thereby allowing for an unlimited source of any cell type. While they are widely used for developing medications and disease modeling, further research must be done to refine the reprogramming process.
- Mesenchymal Stem Cells (MSCs): MSCs can differentiate into several types of cells. Their self-renewal capabilities are far-reaching, making them an ideal candidate for therapies involving tissue repair. They may also be leveraged for cell transplantation in the treatment of neurodegenerative diseases.
- Neural Stem Cells (NSCs): NSCs are derived from specific areas of the brain and are therefore specialized cells. They, too, are self-renewing and multipotent.
Types of Neurodegenerative Conditions Regenerative Medicine can Help Manage:
While researchers are uncovering new findings on how stem cells can treat neurodegenerative conditions nearly every day, there has already been progress. Here are some of the conditions stem cell therapy has been used to manage:
- Parkinson’s Disease (PD): One hallmark characteristic of PD is the decline of dopamine, caused by the destruction of dopamine-producing brain cells. As dopamine decreases, symptoms such as muscle tremors, challenges with movement, and difficulty thinking arise. Now, researchers have found that stem-cell-derived dopaminergic neurons — in particular, those created through ESCs and iPSCs — could hold success in replacing the destroyed brain cells in individuals with PD.
- Alzheimer’s Disease: Through the use of stem cell therapy, researchers at Columbia University have refined the protocol for a unique process of converting skin cells into brain cells. This option streamlines the process of creating neurons to replace those which have become damaged by Alzheimer’s disease. In their research, the cells were able to receive signals just as normal neurons would.
- ALS: ALS has proven remarkably challenging to study, as there are many potential causes and therapies may therefore only be effective on specific patient populations. Moreover, the motor neurons, which are directly impacted by the condition, couldn’t be acquired in large enough numbers to study. Now, however, Harvard researchers have been able to derive mature cells that can be manipulated back into stem cells from ALS patients, opening up new doors for studying potential therapies to treat the condition.
While there is more ground to cover before stem cell therapy for neurodegenerative conditions can become mainstream, promising research is consistently being published. Moving forward, it’s likely that stem cells will hold the answer to viable management options for these and other challenging conditions.

by admin | Oct 29, 2021 | Mesenchymal Stem Cells, Neurodegenerative Diseases, Stem Cell Research, Stem Cell Therapy
Neurodegenerative diseases affect over 50 million Americans each year and occur as a result of nerve cells in the brain, peripheral nervous system, and the central nervous system slowly and progressively losing function before eventually dying[1].
Although there are over 600 known neurological disorders, the most common neurodegenerative diseases continue to be Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and Amyotrophic lateral sclerosis (ALS).
While significant progress has been made in identifying mechanisms and risk factors contributing to the cause and development of these various neurodegenerative diseases, evidence continues to indicate that many of these conditions are influenced by oxidative stress. Research has also shown that antioxidants, the only strategy used to address this mechanism to date, have been demonstrated to be ineffective and, in some instances, even causing additional side effects.
In addition, although progress has been made in the overall understanding and management of several side effects associated with conditions contributing to neurodegeneration and that multifactor intervention introduced at an early stage is believed to be most successful, research has yet to identify a way to slow the progression of these debilitating conditions.
As part of this review, Angeloni et al. provide an analysis of recent literature examining the role of oxidative stress in several neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, ALS, retinal ganglion cells, and ataxia. The authors also discuss the emerging role of mesenchymal stem cells (MSC) and their potential in fighting oxidative stress and enhancing antioxidant capacity and neurotrophin expression.
Recent literature concludes that oxidative stress has a significant role in each of the neurodegenerative diseases mentioned above. Specifically, oxidative stress has been found to:
- Play a fundamental role in Alzheimer’s disease, affecting different pathways involved in AD brain cells.
- Have a causal role and also be a result of different pathologies in PD.
- Be both a cause and consequence of impaired function related to ALS.
- Be a significant cause of damage in a number of ocular neurodegenerative diseases, including diabetic retinopathy, glaucoma, and retina ischemia-reperfusion injury.
- Increase ROS production linked to mitochondrial dysfunction in ataxia cell models.
The literature also indicates that MSC therapy can be a promising future management tool for neurodegenerative disease that enhances antioxidant capacity, increases neurotrophin expression, inhibits pro-inflammatory cytokine secretions, and counteracts microglial ROS production.
However, the authors also conclude that while the role of MSCs in counteracting oxidative stress-related neurodegeneration, additional studies demonstrating a more neurodegenerative disease-specific therapeutic MSC strategy for preventing a broad range of previously mentioned disorders are needed.
Accordingly, these future studies will be useful in helping to discover the appropriate numbers of MSCs needed for transplantation, realize optimal timing of transplantation, identify the correct disease stage for transplantation, and better understand the safety, functionality, recovery, and motor and cognitive improvements of various MSCs used in this process.
Source: (2020, May 7). Role of Mesenchymal Stem Cells in Counteracting Oxidative Stress …. from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7246730/
[1] “Neurodegenerative Diseases: An Overview of Environmental Risk ….” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1280411/. Accessed 18 Oct. 2021.

by Stemedix | May 3, 2021 | Neurodegenerative Diseases, Stem Cell Therapy, Traumatic Brain Injury
In neurodegenerative conditions and cases of brain damage such as traumatic brain injury (TBI), the goal of treatment is usually to manage symptoms and prevent or slow the rate of further damage. Yet, ongoing research suggests stem cells could play an important role in creating new neurons, potentially resulting in repair of central nervous system damage and potentially regrow brain tissue. While the science is still in its infancy, there is evidence to suggest stem cell therapy could help to potentially restore lost brain function.
Just until a couple decades ago, scientists were under the impression that the brain and spinal cord could not rebuild themselves once cells were lost. Yet, in the mid-1990s, neuroscientists discovered that the brain could create new neurons in certain circumstances, which arise from neural stem cells. As undifferentiated cells, the stem cells could give rise to many different brain cell types, including neurons, which carry messages throughout the nervous system.
Further research has supported the idea that neurons can regenerate. For instance, in 2003, research was published which showed improvements in paralyzed rats who were exposed to a virus which caused symptoms similar to that of amyotrophic lateral sclerosis (ALS). Mice that had been previously paralyzed were able to regain some mobility after receiving stem cell injections, and the stem cells took on the characteristics of mature motor neurons.
Researchers have also been exploring stem cell therapies to help treat Parkinson’s disease. The goal is to rebuild the central nervous system through stem cell implantation. While levodopa is the go-to treatment to help regulate dopamine levels which are affected in PD, the drug’s efficacy tends to wear off over time, and its side effects increase. Some researchers have investigated the use of fetal stem cell tissue for PD patients, but lack of standardization and challenges in acquiring donor tissue have been barriers to ongoing research efforts.
With that said, stem cells from umbilical cord blood and adult adipose (fat) or bone marrow can also be coaxed to display many protein markers similar to those found in nervous system cells. It’s unclear whether these cells will ultimately be able to give rise to functioning neurons, but researchers continue to make progress.
Ultimately, there is much left to discover when it comes to the potential role of being able to regrow brain tissue and regenerative therapies such as stem cells in neurodegenerative conditions and brain injury. What we’ve already seen is promising, however. As experts continue to develop a deeper understanding of how stem cells and neurons can work together, patients with these challenging conditions will likely continue to benefit from evolving treatment options. If you would like to learn more then contact a care coordinator today!


 St. Petersburg, Florida
St. Petersburg, Florida
