
by admin | Dec 7, 2018 | Studies, Mesenchymal Stem Cells, Umbilical Stem Cell
Liver failure is a serious, potentially fatal condition in which large swaths of liver cells become dysfunctional and die. Liver failure is the result of several conditions including chronic alcohol consumption, exposure to drugs that are toxic to the liver (e.g. acetaminophen), autoimmune diseases, or infections such as hepatitis C. Liver failure causes several metabolic abnormalities including dangerously low levels of sodium, potassium, and phosphate in the blood. Moreover, four in 10 people with liver failure have trouble regulating their blood glucose levels, which can cause profound hypoglycemia. Since the liver detoxifies the blood, when the liver fails, patients can experience confusion from excessive amounts of ammonia and other substances in the blood. Seizures are also possible.
Short of liver transplantation, there are very few treatments for liver failure. Most treatments focus on restoring sodium, potassium, phosphate, and glucose levels in the blood, and bringing down ammonia levels. Fortunately, experiments show that human mesenchymal stem cells may be a promising treatment for liver failure.
Researchers enrolled 43 people with acute-on-chronic liver failure caused by hepatitis B infection. In this group, 24 patients were treated with mesenchymal stem cells derived from human umbilical cord and 19 patients received a saline solution. The groups received stem cells or placebo, respectively, three times every four weeks. Patients treated with mesenchymal stem cells showed better measures of liver function than those who received placebo. Livers of the patients treated with stem cells produced much more protein, albumin, and clotting factors, and were better able to process bilirubin. Importantly, no significant side effects were observed during the trial.
Given the serious nature of liver failure and the lack of effective treatments (besides liver transplant), this research is incredibly exciting. It offers hope that through further research scientists will be able to use mesenchymal stem cells to change the outcomes of people with acute-on-chronic liver failure.
Reference: https://stemcellsjournals.onlinelibrary.wiley.com/doi/abs/10.5966/sctm.2012-0034

by admin | Nov 28, 2018 | Stem Cell Therapy, Wharton's Jelly
Perinatal stem cells have been attracting attention globally in recent years due to their potential in regenerative medicine. These stem cells come in many forms, due to the wide variety of potential sources for these cells. Perinatal stem cells, for instance, may be umbilical cord-derived hematopoietic stem cells, amniotic epithelial cells, amniotic fluid stem cells, or chorionic mesenchymal stem cells. All sources, nonetheless are considered biological waste and are therefore usually discarded after delivery of babies.
Importantly, perinatal stem cells, despite their origin, tend to share a number of characteristics that make them beneficial in treating conditions. Additionally, unlike other sources of stem cells, retrieval of perinatal stem cells is noninvasive and does not require the ethical considerations that retrieval from other sources may involve. A recent review in Regenerative Medicine has highlighted the potential benefits of perinatal stem cells in therapeutic interventions.
In addition to the relatively easy collection and preparation of perinatal stem cells, these cells tend to be easily harvested and manipulated without harming either the mother or the baby. Upon collection, these stem cells exist in high volume and have greater ability to proliferate than other stem cell types such as bone marrow stem cells. Research has also shown that these cells tend not to lead to adverse immune reactions, though the mechanisms involved in their relationship to the immune system are not well understood.
Given their relative advantages over other stem cell types, perinatal stem cells are well poised to be used in cell-based therapies targeting a wide variety of conditions. Future research will help to define the precise role these cells can play in regenerative medicine and which conditions they may be most useful for.

by admin | Oct 4, 2018 | Stem Cell Therapy, Lupus, Wharton's Jelly
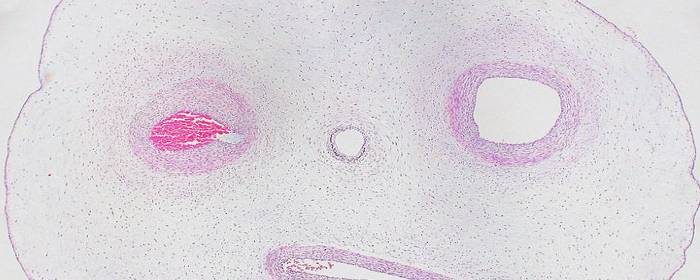
Wharton’s jelly is a rather unique body fluid. It is the connective tissue found within the umbilical cord. While Wharton’s jelly is connective tissue, it more closely resembles gelatin. Historically this material was discarded as medical waste; however, Wharton’s jelly has been shown to contain a number of therapeutic substances. Among these healing substances found within Wharton’s jelly is an abundant supply of mesenchymal stem cells.
One of the most intriguing features of Wharton’s jelly is that it contains a virtually limitless supply of mesenchymal stem cells. There are about 4 million new births in the United States each year, 5 million in the European Union, and over 100 million worldwide. The potential pool of cells is staggering when you consider only a small amount of Wharton’s jelly can contain millions of stem cells. Notably, Wharton’s jelly is usually discarded after the delivery of a healthy baby. If this material could be donated instead of discarded, researchers believe they have found an abundant, renewable resource from which to draw mesenchymal stem cells.
However, the abundance of Wharton’s jelly is not the most impressive feature of the substance. The stem cells found in Wharton’s jelly are rather unique. Perhaps most importantly, the cells are immuno-privileged. This means they are not readily recognized by the immune system. Consequently, the stem cells can be taken from the umbilical cord, purified, and then injected into a patient with little risk of the patient having an immune reaction to the cells. These particular mesenchymal stem cells are also interesting because they are relatively “primitive,” which means they have some of the same properties of embryonic stem cells. However, Wharton’s jelly can be obtained without controversy, while harvesting embryonic stem cells from aborted tissue remain highly controversial.
Stem cells taken from Wharton’s jelly are already being used in some clinical studies. For example, researchers in one clinical study injected type 2 diabetes patients with Wharton’s jelly-derived mesenchymal stem cells. Within six months of treatment, 7 of 22 patients became insulin-free and 5 were able to reduce the amount of insulin they needed by more than 50%. Only one patient out of the 22 did not respond to the stem cells at all. The cells have also been tested in systemic lupus erythematosus, better known as simply lupus. Forty patients received Wharton’s jelly mesenchymal stem cells intravenously. Thirteen patients enjoyed a major clinical response while 11 enjoyed a partial clinical response of their lupus symptoms.
As more clinical studies are done on Wharton’s jelly-derived mesenchymal stem cells, we will learn what other diseases can be treated with this once-discarded substance. Early indications show a very promising future.

by admin | Oct 14, 2017 | Stem Cell Research
Research into stem cell-based therapies has increased in recent years due to observations that these types of cells can provide new avenues for treatment where other treatment options are limited. Though bone marrow mesenchymal stem cells have been the gold standard of stem cell-based therapies, there is mounting evidence that umbilical cord stem cells may offer some advantages over bone marrow mesenchymal stem cells, as well as other popular stem cell types, such as adipose tissue, periodontal ligament, and dental pulp. In a recent review in Tissue Engineering, Reine El Omar and colleagues describe the state of umbilical cord stem cell research and the potential benefits of using these cells in stem cell therapies.

According to Omar et al., umbilical cord-derived stem cells were once thought of as medical waste. However, they have now been shown to provide advantages over other stem cells in stem cell-based therapies in 3 major ways:
- Umbilical cord stem cells are easier to collect than are other stem cell types. Extracting bone marrow mesenchymal stem cells, for instance, is technically difficult and painful for donors. Umbilical cord stem cells can be painlessly collected and banked.
- Stem cells tend to proliferate more than other stem cells types. Other stem cell types have been shown to have limited proliferation and differentiation potential. Umbilical cord stem cells, on the other hand, appear to be more proliferative and differentiate longer.
- Umbilical cord stem cells are associated with less severe immune reactions than are other stem cells types. A critical aspect of the practicality of stem cells is their ability to act as therapeutic agents without causing adverse reactions. When the immune system perceives stem cells as dangerous foreign agents, the immune system can react in dangerous ways that lead to tissue damage and even death. Compared to other types of stem cells, umbilical cord stem cells appear to be associated with less severe immune reactions.
While efficacy is important for stem cell-based therapies, safety is perhaps more critical. Thus, research into how stem cells can be used therapeutically must focus not only on what therapeutic impact these cells can have but also what risks these cells pose. Future research will help to determine the safest cells to use and how those cells can best be incorporated to achieve their therapeutic goals.
Learn more about stem cell treatments here.
Reference
Omar et al. (2014). Umbilical cord mesenchymal stem cells: The new gold standard for mesenchymal stem cell-based therapies?

by admin | Aug 7, 2017 | Studies
A recent review in the World Journal of Stem Cells has described the nature of umbilical cord-derived mesenchymal stem cells and the clinical advantages of using these stem cells over other types of stem cells. Other mesenchymal stem cells that are used in research come from: bone marrow, peripheral blood, cord blood, placenta, adipose tissue, dental pulp, and fetal liver and lungs.
One of the main advantages of umbilical cord stem cells, for both research and clinical purposes, is its ease of collection. The collection is noninvasive, circumventing the issue of causing pain to extract the cells. Further, as umbilical cord is generally viewed as medical waste, the cells can be collected without the same ethical issues that are raised by the collection of other cell types.
The cells are also plentiful when collected and can be banked for later use. According to the researchers, the only disadvantage of umbilical cord stem cells in this context is that a physician must evaluate the baby donor’s health and confirm that the cells derive from a healthy baby. This requirement stems from the fact that the cells are more likely to develop into healthy cells themselves if they come from a healthy baby. However, in the case of bone marrow-derived mesenchymal stem cells, a physician can evaluate the potential donor first and then decide whether to collect the cells.
The immunomodulatory characteristics of umbilical cord-derived mesenchymal stem cells also represent a major practical advantage of these cells for clinical applications. The introduction of any foreign agent to the body poses a risk because the immune system may recognize the matter as foreign and deem it threatening. If this immune response occurs, the immune reaction that ensues can cause severe long-term damage to tissues. Given that umbilical cord-derived mesenchymal stem cells cause these immune reactions much less frequently than do other stem cell types makes them potentially safer as therapeutic interventions.
More research is needed to determine the best ways to use umbilical cord-derived mesenchymal stem cells. However, the evidence that there are clinical benefits to using these cells over other stem cell types is accumulating.
To learn more about the five benefits of stem cell therapy, click here.
Reference
Nagamura-Inoue & He, H. (2014). Umbilical cord-derived mesenchymal stem cells: Their advantages and potential clinical utility. World Journal of Stem Cells, 6(2), 195-202.


 St. Petersburg, Florida
St. Petersburg, Florida
