
by admin | Dec 2, 2019 | ALS, Bone Marrow, Stem Cell Research, Stem Cell Therapy
Researchers have recently established that a hallmark of Amyotrophic Lateral Sclerosis (ALS) is endothelial cell degeneration that leads to vascular pathology. When this vascular pathology occurs, damage develops to the barrier between the blood and the central nervous system. Given this new understanding of the pathophysiology of ALS, researchers have begun looking at the potential of repairing this barrier as a strategy for treating the disease with bone marrow stem cells.
A recent study, published in Scientific Reports, addressed this issue by testing how human bone marrow cells may impact blood-spinal cord barrier repair by transplanting these cells in an ALS model. The researchers hypothesized that the cells should help to repair the barrier, reversing the damage accompanying ALS. They were also interested in whether this type of repair may improve not only the integrity of the barrier between the blood and central nervous system but also improve symptoms of ALS.
What the researchers found was that the human bone marrow cells differentiated into the type of endothelial cells that were needed for repair and successfully engrafted into the capillaries of the spinal cord in their model. Several specific observations led the scientists to conclude that these stem cells helped to effectively restore the barrier between the blood and the spinal cord.
The stem cells improved the integrity and survival of nervous system cells, including astrocytes and spinal cord motor neurons, preventing problematic changes in these cells that are associated with the breakdown of the blood-central nervous system barrier. Critically, the implantation of the stem cells also led to improvements in behaviors associated with ALS.
While there is still a lot of research to be done to establish whether bone marrow stem cells can help repair the blood-spinal cord barrier in patients with ALS, this study provides promising data. Given that there is no cure for ALS and limited treatment options, there is likely to be an emphasis on cell-based therapies for the disease. As more data become available, we will get a clearer picture as to if and how stem cells can help ALS patients.
Reference: Garbuzova-Davis,S. (2017). Endothelial and astrocytic support by human bone marrow stem cell grafts into symptomatic ALS mice towards blood-spinal cord barrier repair. Scientific Reports, 7(884).

by admin | Aug 16, 2018 | Hyperbaric Oxygen Therapy, Bone Marrow, Stem Cell Research
Stem cells are generating so much excitement in research and clinical circles because they have the capacity to become many other types of cells. They also release a number of important molecules such as hormones, cytokines, and genetic material that can potentially be helpful for patients. Researchers have found that not only does hyperbaric oxygen therapy (HBOT) help in the circulation of stem cells but it also will help to mobilize stem cells from the bone marrow to the bloodstream further preparing the patient for stem cell therapy.
Bone marrow is a rich source of stem cells, but getting them usually requires an invasive procedure, i.e., placing a large bore needle into the middle of bone(s). Researchers have discovered, however, that hyperbaric oxygen treatment causes stem cells from the bone marrow to move into the bloodstream by specifically stimulating the body’s nitric oxide synthesis. Thus, instead of using a needle to extract stem cells from the bone marrow, patients can potentially increase their own bone marrow stem cells by undergoing hyperbaric oxygen treatment.
Stephen Thom, MD, Ph.D. and co-researchers at the University of Pennsylvania showed that a single hyperbaric oxygen treatment could double the number of bone marrow stem cells in the blood. This means that the hyperbaric oxygen was “mobilizing” the stem cells to move from the bone marrow into the bloodstream to allow them to move into areas of the body that benefit from them. Moreover, when study subjects underwent 20 treatments of hyperbaric oxygen therapy over a few weeks, the number of bone marrow stem cells in the blood increased significantly by eightfold. This astonishing finding has been confirmed in subsequent experiments.
The most important conclusion from this research is that hyperbaric oxygen therapy treatments can unlock the potential of a person’s own bone marrow stem cells without an invasive procedure. While many scientists assumed that the benefits of hyperbaric oxygen therapy were due to the high concentrations of oxygen infusing the blood, tissues, and cells, they now have research to support that these benefits may also be due to stem cell mobilization.

by admin | Aug 10, 2018 | Bone Marrow, Wharton's Jelly
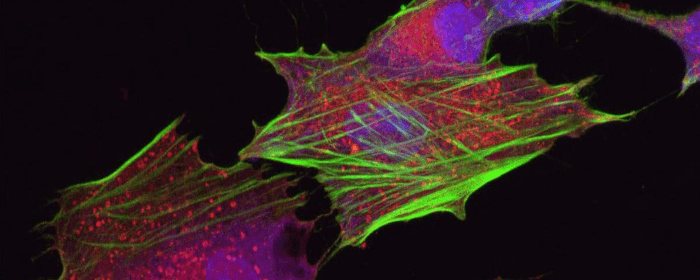
Mesenchymal stem cells that come from different cell sources can look similar but behave differently. Bone marrow-derived mesenchymal stem cells tend to be the gold standard for isolating and using mesenchymal stem cells, it is not particularly easy to access these cells from the bone marrow. Because there are other, much more easily accessible mesenchymal stem cells, such as those from the umbilical cord, it is important to establish the differences between the different types of stem cells so that each can be used when most appropriate and when most advantageous.
One important difference is how to isolate the cells and how easy it is to do so. Recent work published this year in Stem Cells and Development helped to define the best way to isolate mesenchymal stem cells from the Wharton’s jelly of umbilical cords. The researchers also looked at the gene expression profile and the immune system characteristics of both bone marrow-derived mesenchymal stem cells and Wharton’s jelly-derived mesenchymal stem cells.
The researchers found that mesenchymal stem cells that came from the Wharton’s jelly of the umbilical cord had a better capacity to expand into more tissue than those taken from the bone marrow. Further, their gene expression was different. In the stem cells from the Wharton’s jelly, there was greater gene enrichment for genes related to cell adhesion, proliferation, and immune system functioning than in the cells from the bone marrow. These cells also induced the maturation of brain cells more so than did the mesenchymal stem cell derived from bone marrow.
These results show that Wharton’s jelly-derived mesenchymal stem cells have distinct properties from bone marrow-derived mesenchymal stem cells and likely have specific advantages as well to help treat those battling osteoarthritis, multiple sclerosis, Parkinson’s disease, and other degenerative conditions. Further research will help bear out more of the differences between these types of stem cells and how each type can best be used to help patients.

by admin | Jul 25, 2018 | Bone Marrow, Health Awareness, Stem Cell Research, Stem Cell Therapy
Stem cells derived from bone marrow, or hematopoietic stem cells, are a topic of significant debate in the medical community. While they have exhibited significant potential for benefiting people with both cancerous and noncancerous diseases including immune deficiencies, not all methods for administering bone marrow are created equal. While intra-articular injections of bone marrow are more common and considered safer, intravenous methods pose serious risks, which are explored here.
Intra-articular injections involve injecting bone marrow directly into the compromised joint, whereas intravenous methods entail infusing bone marrow stem cells into the body through the veins. Intra-articular injections have shown promise in treating conditions such as osteoarthritis (OA) in joints such as the knee and has proven to achieve pain relief for moderate-to-severe cases of osteoarthritis.
Intra-articular treatments are localized, so the injected bone marrow is already in its target location upon being administered. According to research, this form of therapy is generally considered to be safe. In intravenous bone marrow transplants, however, there are serious risks associated with treatment. Bacterial infections are common, while viral and fungal infections can also occur and cause life-threatening conditions, such as organ failure.
Risk factors for developing any complication associated with intravenous bone marrow transplantations vary based on a number of factors, including the patient’s age, genetics, and type of disease being treated. With that said, due to its limited risks, intra-articular bone marrow methods appear to be the safest form of treatment currently available. Although each patient will need to discuss risk factors alongside potential benefits with his or her physician, oftentimes the risks appear to outweigh the potential benefits.
There are alternative therapies with fewer potential side effects which may be explored such as Adipose and Umbilical Cord-derived stem cells. These regenerative medicine treatments not only can treat osteoarthritis and sports-related injury conditions, but have also shown positive results in treating neurological conditions such as Multiple Sclerosis, Parkinson’s disease, Post-Stroke, and Traumatic Brain Injuries (TBI).

by admin | Feb 20, 2017 | Studies
Diabetic patients from deficiencies in insulin, a hormone that is critical for regulating blood sugar levels. Researchers have recently shown how combining mesenchymal stem cells with bone marrow cells can induce the regeneration of cells that secrete insulin and thereby restore normal levels of blood sugar and blood insulin.
The insulin deficiency that occurs in diabetes differs based on the type of diabetes that a patient has. In type 1 diabetes, cells in the pancreas that produce insulin, known as beta-cells, are destroyed, preventing the normal production and secretion of insulin. In type 2 diabetes, however, insulin is still produced and secreted, but insulin sensitivity is reduced, meaning that the body does not respond properly to the presence of insulin in the blood. In both cases, there is a reduction in the number of properly functioning beta-cells.
Previous research has shown that adult bone marrow contains cells that can enhance the regeneration of beta-cells in diabetes. However, the findings have been countered by other studies that have not found this effect. In the current study, researchers aimed to determine whether bone marrow cells that are injected in combination with mesenchymal stem cells could increase the amount of functional beta-cells in diabetes. The scientists were also interested in whether any increase in functional Beta cells that may be observed as a result of this intervention would have the practical effect of restoring normal blood insulin and blood glucose levels in diabetes.
Though injecting just bone marrow cells or just mesenchymal stem cells did not impact beta-cell number or blood insulin or blood glucose levels, the combination of the two did. After a single injection, researchers observed tissue regeneration. Importantly, the new beta-cells were generated by the recipient, as no donor beta-cells were identified in recipients. Thus, the bone marrow cell and stem cell combination did not simply replace cells but instead instigated the regeneration of cells. Further, because blood insulin and blood glucose levels were restored after these injections, the newly generated beta-cells were not only present but also functional.
Another positive outcome of this procedure was that there was no immune response initiated against the new beta-cells, suggesting that these cells could survive in the long-term. These findings show the tremendous promise that stem cells have, especially when strategically combined with other interventions, to diabetes therapy.
Find out how stem cells provide regenerative therapy for Diabetes here.
Reference
Urban, V.S. et al. 2008. Mesenchymal stem cells cooperate with bone marrow cells in therapy of diabetes. Stem Cells, 26, 244-253



 St. Petersburg, Florida
St. Petersburg, Florida
