
by admin | Mar 14, 2019 | Spinal Cord Injury, Stem Cell Research
Traumatic spinal cord injury is a potentially devastating event in which the nerves and nerves cells in the spinal cord are damaged. In the United States, more than a quarter of a million people struggle with the lifelong consequences of traumatic spinal cord injury. The consequences of spinal cord injury vary from person to person, but each person usually must deal with several complications. Many people with spinal cord injury are paralyzed. They are at risk for pressure ulcers, blood clots in the legs, urine and bowel problems, and sexual dysfunction. Despite being paralyzed, as many as two-thirds of patients with spinal cord injury experience chronic pain, which is difficult to treat. Spinal cord injury can also affect how the heart and lungs function.
There are no specific treatments for spinal cord injury. If the injury is treated early, steroids and spine surgery/neurosurgery can help reduce long-term complications. In some cases of incomplete spinal cord injury, physical therapy can help people regain some degree of function. For the most part, treatment is aimed at reducing symptoms rather than curing the injury. Treating the symptoms helps make the disease less of a burden, but is by no means the same as a cure.
Because spinal cord injury has such long-lasting and devastating effects, researchers are actively pursuing ways to heal injured spinal cord nerve cells. One possible way to do this is through the use of stem cells.
Liu and coauthors conducted a clinical trial on 22 patients with spinal cord injury. The doctors collected mesenchymal stem cells from umbilical cord tissue that would normally be discarded as medical waste after delivery. They purified the stem cells and then used them to treat the injured patients. Astoundingly, stem cell treatment was effective in 13 of 22 patients. Patients who achieved benefit from stem cells enjoyed the return of motor function, sensory function, or both. All patients who were treated with stem cells reported less pain, improved sensation, better movement, and a greater ability to provide self-care. Importantly, the treatment did not cause any notable side effects for up to three years after treatment.
These clinical trial results are truly remarkable, but it is important to note that the number of patients treated was small and further testing is needed. Nevertheless, the researchers concluded that treatment with mesenchymal stem cells derived from umbilical cells is safe, and can improve function and quality of life in most patients with spinal cord injury.
Reference: Liu et al. (2013). Clinical analysis of the treatment of spinal cord injury with umbilical cord mesenchymal stem cells. Cytotherapy. 2013 Feb;15(2):185-91.

by admin | Mar 1, 2019 | Mesenchymal Stem Cells, Osteoarthritis, Stem Cell Therapy, Studies
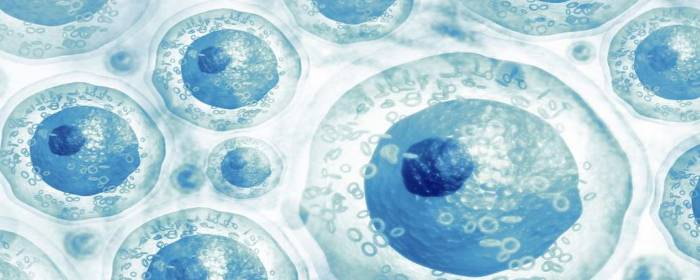
Cartilage plays several important roles in the way joints move and function. Joint cartilage provides lubrication, acts as a shock absorber, and helps the joint move smoothly. Joint cartilage is comprised of two substances chondrocytes (i.e. cartilage cells) and extracellular matrix (proteins such as hyaluronic acid, collagen, fibronectin, etc.).
Many conditions can lead to joint cartilage defects. In young people, the most common cause of the joint cartilage defect is an injury. For instance, a football player suffers a hard contact that injures the joint. Another example is a gymnast who repeatedly places substantial impact forces on the knee and other joints of the lower body, resulting in damage. In older people, the most common cause of joint cartilage defects is Osteoarthritis. Over time, the joint cartilage breaks down in the cartilage loses its ability to lubricate, absorb shock, and support the smooth movement of the joint. This leads to stiffness, pain, and “trick” joints, among other symptoms.
Orthopedic surgeons, rheumatologists, and other physicians have attempted to treat these conditions by injecting the damaged joint with one of the two main components of joint cartilage: extracellular matrix. Physicians inject hyaluronic acid (and sometimes related extracellular matrix proteins) to help replace and restore damaged joints. This approach can be helpful for some patients, but it is certainly not a cure.
Only recently, have researchers attempted to replace the other component of joint cartilage: chondrocytes. Specifically, researchers have focused their efforts on mesenchymal stem cells that have the ability to differentiate and become cartilage cells. Li and colleagues injected combinations of bone marrow-derived mesenchymal stem cells and hyaluronic acid into animals with experimental cartilage defects. They showed that hyaluronic acid injections alone modestly repaired the cartilage damage. However, when stem cells plus hyaluronic acid was injected, the joints were almost completely repaired. In other words, stem cells plus hyaluronic acid resulted in much greater improvement in joint cartilage damage than hyaluronic acid alone.
The authors of the study concluded that “bone marrow stem cells plus hyaluronic acid could be a better way to repair cartilage defects.” While additional work is needed, these results are extremely exciting for people who suffer from joint cartilage defects such as osteoarthritis. In the future, people who are candidates for hyaluronic acid injection treatments may instead receive a combination of hyaluronic acid plus stem cells and may enjoy an even greater benefit than hyaluronic acid treatment alone.
Reference: Li et al. (2018). Mesenchymal Stem Cells in Combination with Hyaluronic Acid for Articular Cartilage Defects. Scientific Reports. 2018; 8: 9900.

by admin | Feb 1, 2019 | Adipose, Exosomes, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Studies, Umbilical Stem Cell
Most organs of the body recover from injury by generating new, healthy cells. Not every organ of the body has the same ability to form new cells, however. The skin is an example of an organ that has an amazing ability to regenerate. Liver and lung also have the ability to form new cells, but not as dramatically as skin. Kidney and heart have even less ability to repair and regenerate. On the opposite end of the spectrum from the skin is the brain, which has very little capacity to regenerate once it has been damaged or destroyed. All of these organ systems, especially those that are relatively unable to repair themselves, could theoretically benefit from stem cells.
Mesenchymal stem cells, also known as stromal cells, are multipotent stem cells derived from bone marrow, umbilical cord, placenta, or adipose (fat) tissue. These cells can become the cells that make up bone, cartilage, fat, heart, blood vessels, and even brain. Mesenchymal stem cells have shown a remarkable ability to help the body to produce new cells. Researchers are now realizing that the substances stem cells release may be more important than any new cells they may become. In other words, stem cells can directly become new healthy cells to a certain degree, but they can also release substances that dramatically increase the number of new, healthy cells.
Mesenchymal stromal stem cells release small packets called exosomes. These exosomes are filled with various substances that promote cell and tissue growth. Some of the most interesting and potentially useful substances are cytokines and micro RNA. Cytokines are the traffic cops of cellular repair, signaling certain events to take place while stopping others. Having the right cytokines in a particular area is critical for new tissue growth. The micro RNA released by stem cell exosomes is potentially even more exciting than cytokines. These tiny bits of RNA can directly affect how healthy and diseased cells behave. Micro RNA has a powerful ability to control the biological machinery inside of cells.
Exosomes exhibit a wide array of biological effects that promote the repair and growth of damaged and diseased organs. They promote the growth of skin cells and help wounds heal. Exosomes can reduce lung swelling and inflammation and even help the lung tissue heal itself (i.e. reduced pulmonary hypertension, decrease ventricular hypertrophy, and improve lung vascular remodeling). These small packets released by stem cells help prevent liver cells from dying (i.e. prevents apoptosis), promote liver cell regeneration, and slow down liver cirrhosis (i.e. fibrosis). Exosomes can also help protect the kidneys during acute injury and reduce the damage that occurs during a heart attack.
Several clinical trials are underway designed to allow these exciting developments to be used to treat patients. As the researchers state, “Extensive research and clinical trials are currently underway for the use of MSCs as regenerative agents in many diseases including spinal cord injury, multiple sclerosis, Alzheimer’s disease, liver cirrhosis and hepatitis, osteoarthritis, myocardial infarction, kidney disease, inflammatory bowel disease, diabetes mellitus, knee cartilage injuries, organ transplantation, and graft-versus-host disease.” We can reasonably expect that exosomes will be used to treat at least some of these conditions in the very near future.
Reference: Rani al. (2015). Mesenchymal Stem Cell-derived Extracellular Vesicles: Toward Cell-free Therapeutic Applications. Molecular Therapy. 2015 May; 23(5): 812–823.

by admin | Jan 27, 2019 | Exosomes, Heart Failure, Kidney Disease, Stem Cell Research, Stem Cell Therapy, Stroke, Umbilical Stem Cell
Tissue injury is common to many human diseases. Cirrhosis results in damaged, fibrotic liver tissue. Idiopathic pulmonary fibrosis and related lung diseases cause damage to lung tissue. A heart attack damages heart tissue, just as a stroke damages brain tissue. In some cases, such as minor tissue injury, the damaged tissue can repair itself. Over time, however, tissue damage becomes too great and the organ itself can fail. For example, long-standing cirrhosis can cause liver failure.
One area of active research is to find ways to protect tissue from injury or, if an injury occurs, to help the tissue repair itself before the damage becomes permanent and irreversible. Indeed, tissue repair is one of the main focuses of regenerative medicine. Likewise, one of the most promising approaches in the field of regenerative medicine is stem cell therapy. Researchers are learning that when it comes to protecting against tissue injury and promoting tissue repair, exosomes harvested from stem cells are perhaps the most attractive potential therapeutic.
Why are stem cell exosomes so promising? Exosomes are small packets of molecules that stem cells release to help the cells around them grow and flourish. While one could inject stem cells as a treatment for diseases (and they certainly do work for that purpose) it may be more effective in some cases to inject exosomes directly. So instead of relying on the stem cells to produce exosomes once they are injected into the body, stem cells can create substantial amounts of exosomes in the laboratory. Exosomes with desired properties could be concentrated and safely injected in large quantities, resulting in a potentially more potent treatment for the disease.
Indeed, researchers have shown that extracellular vesicles (exosomes and their cousins, microvesicles) can be collected from stem cells and used to treat a variety of tissue injuries in laboratory animals.
Just a few examples of this research:
- Exosomes from umbilical cord-derived mesenchymal stem cells were able to accelerate skin damage repair in rats who had suffered skin burns.
- Exosomes from the same type of stem cell protected the lungs and reduced lung blood pressure in mice with pulmonary hypertension.
- Exosomes from endothelial progenitor cells protected the kidney from damage caused by a lack of blood flow to the organ.
In this growing field of Regenerative Medicine, research is constant and building as new science evolves from stem cell studies. Researchers are closing in on the specific exosomes that may be helpful in treating human diseases caused by tissue injury.
Reference: Zhang et al. (2016). Focus on Extracellular Vesicles: Therapeutic Potential of Stem Cell-Derived Extracellular Vesicles. International Journal of Molecular Sciences. 2016 Feb; 17(2): 174.

by admin | Jan 15, 2019 | Exosomes, Mesenchymal Stem Cells, Stem Cell Research, Studies
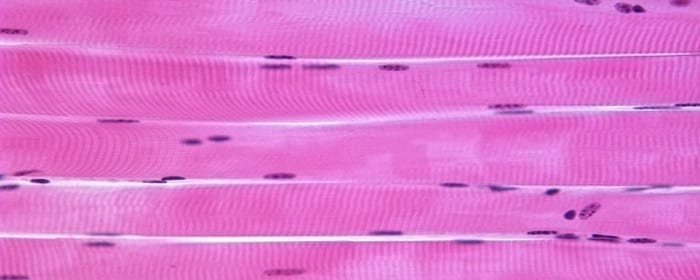
Muscle health and strength is an important determinant of a person’s ability to function in daily life. One of the major determinants of healthy aging is how well people retain their muscle mass. The more that skeletal muscle declines, the more likely someone would not be able to care for themselves independently. Injury to muscles whether through trauma, burns, or toxins can greatly interfere with a person’s ability to perform activities of daily living. While muscle cells have a limited ability to regenerate themselves, quite often, patients never regain their former strength and level of function after serious injury.
Stem cells would seem to be ideally suited to help in this regard. Since stem cells have the potential to become muscle cells, one could imagine infusing stem cells into an area of muscle damage or injury to restore overall muscle function. While this makes sense intuitively, it may not be the case. Stem cells, for example, form new muscle cells, but they do not form cells that participate in muscle function. And yet, stem cells are able to help muscles regrow into functional skeletal muscles.
How could stem cells promote skeletal muscle regeneration without becoming functional skeletal muscle cells? The answer, as it turns out, is that stem cells produce molecules that strongly promote muscle regeneration and muscle function.
Stem cells release these molecules in tiny packets called exosomes. Exosomes are tiny spheres that “bubble out” of stem cells, in a manner of speaking. Exosomes have a cell membrane, like cells themselves, but are much smaller, and they do not have the ability to reproduce. Instead, exosomes are highly packed with proteins, DNA, messenger RNA, micro RNA, cytokines, and other factors.
Nakamura and co-researchers showed exosomes can help regenerate muscle. These researchers showed that by injecting exosomes harvested from stem cells (without any of the stem cells themselves), they could increase muscle growth and blood vessel growth. In short, these molecules accelerate the rate at which muscles regenerate.
While more research is needed, this work suggests that exosomes retrieved from mesenchymal stem cells could be used to help regrow functional muscle in patients with various forms of muscle injury.
Reference: Nakamura et al. (2015). Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. FEBS Letters. 2015 May 8;589(11):1257-65.


 St. Petersburg, Florida
St. Petersburg, Florida
