
by admin | Apr 13, 2022 | Health Awareness, Multiple Sclerosis
Muscle spasticity is one of the most challenging symptoms of Multiple Sclerosis (MS). Patients with MS often experience a tightening or stiffening of the lower body muscles in the legs, groin, buttocks, and back.
Muscle spasticity can affect the ability to stand, walk, and balance and is one of the biggest detriments to a patient’s quality of life. Muscle spasticity can worsen during quick stretches or movements. However, when done correctly, gentle stretches can help patients manage spasticity effectively.
Hip Crossovers
While lying on your back, bend your knees at a 45-degree angle, draw them together, and gently let both knees lower to one side, holding for 30 seconds. Then pull the knees back to the center and slowly lower them to the other side.
In this hip stretch, your goal is to decrease tightness, not get your knees to the floor, so only lower them as far as it feels okay. Keep your arms out to the side in a “T,” palms down. Move slowly.
Hip Flexor Stretches
Lying on your back, rest on the lower half of your bed with your knees and lower legs hanging off the edge. You should feel a stretch in your hip flexors located at the front of your hip. Aim to build up to a 30-second, then 60-second hold.
Calf Stretches
Placing a rolled-up towel on the floor, step on the towel with the ball of your foot, keeping your weight on the back of the foot. Then, step the opposite foot slightly forward, still maintaining the weight on the back of the foot, stretching the calf.
Foot Rolls
When seated, place a rubber ball on the floor and roll your foot over the ball, paying particular attention to places on your foot that lack feeling or feel disengaged.
Ankle Stretches
While seated, hold a rolled towel at both ends, wrapping the towel under one foot. Lift the foot and towel with both hands and try to keep the leg extended for up to 30 seconds.
Tips for Exercising with Muscle Spasticity
Muscle spasticity affects everyone differently. If you experience muscle spasticity when extending your legs, avoid stretches that straighten the knee and hip to that point. Also, patients who incorporate stretches regularly see the most benefits and better movement.
If you take an anti-spasticity drug, exercise about an hour after taking your medication, and have your dosage checked regularly as spasticity changes.
If your spasticity worsens, or you’re not finding relief from the suggested exercises, schedule time with a physical therapist to learn about the best exercises for your needs.

by Stemedix | Apr 11, 2022 | Parkinson's Disease, Mesenchymal Stem Cells, Stem Cell Therapy
Regenerative medicine, also known as stem cell therapy, is emerging as a viable treatment for Parkinson’s disease as clinical trials move through the FDA approval process. Patients in clinical trials see positive results from mesenchymal stem cell therapy for Parkinson’s Disease.
What Is Parkinson’s Disease?
Parkinson’s disease is a progressive, neurodegenerative condition. It occurs when dopamine-producing brain cells stop working or die. Dopamine’s role in the body is to send messages between nerve cells or from nerve cells to muscle cells, affecting the body’s physical and mental functions.
Symptoms of Parkinson’s start gradually, and the disease worsens over time. Early symptoms include tremors in the hands, rigidity, and slowness of movement. Patients with Parkinson’s also experience difficulty with balance, and eventually, with speech, writing, and automatic muscle movement such as blinking.
While there’s currently no cure for Parkinson’s, there are medications that patients can take to manage symptoms. Some symptoms are also relieved from surgery to regulate specific brain areas.
Patients with Parkinson’s disease experience a progressive decline in their ability to function, with treatments only offering some relief. The emergence of mesenchymal stem cell therapy as an option to reverse the damage and halt the progression of Parkinson’s disease is an exciting development.
What Are Mesenchymal Stem Cells?
Stem cells are considered to be the building blocks of cells. All specialized cells in the body come from stem cells. When stem cells divide, they either produce more stem cells, called daughter cells, or differentiate into specialized cells, such as bone, blood, or brain cells.
Mesenchymal stem cells (MSCs) are adult stem cells commonly found in bone marrow. They also exist in adipose (fat), umbilical cord tissue, amniotic fluid, and other locations. MSCs remain dormant in the bone marrow until they’re needed to facilitate healing in the body.
MSCs differentiate into:
- Bone cells
- Muscle cells
- Skin cells
- Cartilage
- Neural cells
- Corneal cells
MSCs are present throughout your life, but they age as the body ages, making them less effective and concentrated over time.
How Can Mesenchymal Stem Cells Benefit Those with Parkinson’s Disease?
In recent clinical trials using mesenchymal stem cells on Parkinson’s patients, the cells significantly improved patients’ symptoms, including facial expressions, gait, and rigidity or “freezing” episodes. Some of the patients in this study substantially reduced their dosages of medicines used to control Parkinson’s symptoms.
In a 2005 study, researchers determined that stem cells may be capable of differentiating into dopamine neurons, which are damaged or destroyed with Parkinson’s.
While the true potential of mesenchymal stem cell benefits in Parkinson’s patients is still being investigated, there is reason to believe that patients with the neurodegenerative condition could experience a significant improvement in their quality of life with stem cell therapy. If you are interested in learning more about Mesenchymal Stem Cell Therapy for Parkinson’s Disease, contact us today at Stemedix!

by admin | Apr 6, 2022 | Health Awareness
Most people understand what collagen is, but many are not yet familiar with liposomal vitamin C. Both of these substances are beneficial for improving gut health and reducing the inflammation that can cause stiff, swollen joints.
Benefits of Collagen
Collagen is a protein found naturally in the human body. In fact, it is the most abundant protein in the body. It is located in the musculoskeletal system, in blood vessels, and also in the digestive system.
It is often thought of as the “glue” that holds the body together. Even before the age of 30, most people have started losing their collagen stores. By 40, it is depleting more quickly than we can produce it.
Though it is mostly known for keeping skin youthful, collagen is vital in maintaining a healthy digestive system. It helps repair leaky gut by sealing the intestines and protecting them from toxins in the digestive tract.
Collagen is necessary to “heal, seal, and repair” the gut lining and return the digestive system to its natural balance.
Benefits of Liposomal Vitamin C
Liposomes are “nano-sized” transporters. They are responsible for carrying nutrients directly from the blood to the body’s cells. Liposomal vitamin C is a type of vitamin C that is more easily absorbed by the body. Microscopic droplets of fat-soluble liposomes encapsulate the vitamin C, making it easier to transport and access.
Nearly 80% of water-soluble vitamin C is excreted from the body, but almost 90% of liposomal vitamin C is directly absorbed into the digestive tract cells.
Liposomal vitamin C is easier on the gut and may help reduce the GI symptoms related to taking high doses of water-soluble vitamin C. Vitamin C is an important supplement for reducing inflammatory markers. It has effectively reduced the inflammatory symptoms associated with colds, flu, and seasonal allergies.
For more health awareness blogs, please visit www.stemedix.com/blog.

by admin | Apr 1, 2022 | Stem Cell Therapy, Adipose, Mesenchymal Stem Cells, Musculoskeletal, Wharton's Jelly
Articular cartilage, found on the surface of most musculoskeletal joints, distributes and transfers forces between bones and joints, provides a smooth surface for joint mobility, and plays an important role in human mobility.
However, articular cartilage is also easily susceptible to damage, but difficult to repair itself on its own (primarily due to the fact it is mostly avascular). Over time, the inability of articular cartilage to repair itself leads to progressive joint pain, disfigurement, movement disorders, and ultimately osteoarthritis.
The CDC estimates that nearly 33 million Americans are currently affected by osteoarthritis, most often in the form of pain, stiffness, decreased mobility and range of motion, and swelling in the joints[1].
Current treatment methods, including microfracture technology, autologous or allogeneic cartilage transplantation, and autologous chondrocyte implantation (ACI) have demonstrated the ability to repair and regenerate fibrous cartilage, but not articular cartilage required for smooth, fluid, natural mobility.
To address this issue, recent research has focused on the efficacy of stem cells, and specifically mesenchymal stem cells (MSCs) found in bone marrow, adipose tissue, synovial membrane, and umbilical cord Wharton’s jelly, as potential therapeutic treatments for regeneration of articular cartilage. MSCs are particularly of interest due to their demonstrated abilities of self-renewal, multi-differentiation, and immunoregulation.
While the use of MSCs has demonstrated tremendous potential in the field of regenerative therapy, one notable drawback continues to be unstable or suboptimal results resulting from the heterogeneity of various mesenchymal stem cells.
Specifically, the stability and efficacy of MSCs appear to differ based on a number of factors, including the donor, the tissue source, and their ability for proliferation, differentiation, and immunoregulation.
For example, some of the key heterological differences highlighted in this review include the efficacy of MSCs based on donor’s age (with younger donors providing higher quality MSCs), Wharton’s Jelly MSCs showing greater prospects for application in cartilage regeneration than other MSCs, and differences within specific MSC subpopulations.
The authors of this review acknowledge the potential of MSCs in repairing arterial cartilage, but also point out that there needs to be a deeper understanding of the heterogeneity of various MSCs in order to improve the efficiency of MSC-based therapies designed to repair arterial cartilage. In addition, the authors also call for greater standardization in MSC isolation and harvesting methods among laboratories in order to provide better consistency with respect to results obtained from studies using MSCs.
Source: “Heterogeneity of mesenchymal stem cells in cartilage regeneration.” 19 Mar. 2021, https://www.nature.com/articles/s41536-021-00122-6?elqTrackId=5517bd20493b470cb34fd0e8bc1f6ef9.
[1] “Osteoarthritis (OA) | Arthritis | CDC.” https://www.cdc.gov/arthritis/basics/osteoarthritis.htm.

by admin | Mar 30, 2022 | Health Awareness
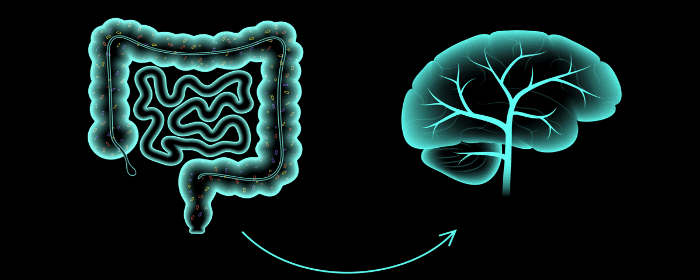
Scientists researching the human gastrointestinal tract’s microorganisms continue to find significant connections between the gut and patients’ overall health.
The gut microbiome, which is the name for these microorganisms, has inspired many studies as researchers continue to understand their impact on everything from brain disorders to joint pain.
While initial studies linking the gut microbiome to cognitive function showed connections, those studies used animal experiments and small clinical studies. On a larger scale, scientists examining the gut microbiome’s relationship to cognitive function recruited middle-aged participants from another study in four U.S. metropolitan areas.
Previous Studies
Previous studies looking at connections between the gut microbiome and cognitive function found links for short-chain fatty acids produced in the microbiota to influence cognitive health.
In animal experiments, rodents with reduced diversity in their gut microbiome showed cognitive defects, including reduced memory, impaired working memory, and changes in their brain.
Small-scale human studies also showed associations between the gut microbiome and cognition, including improvements when comparing controls to people treated with probiotics to increase their gut microbiome.
The Newest Results
In scientists’ newest study, they analyzed the cognitive function and microbiomes of 597 participants between 48 and 60 years old, with a mean age of 55. The study focused on participants’ gut microbiome diversity in connection with six cognitive tests.
The studies concluded a significant association between participants’ microbial composition and cognitive function. All of the conclusions drawn were in line with the previous small-scale human studies and animal studies.
Conclusions
While researchers carefully note that this study needs replication in larger human samples, some of the initial findings support short-chain fatty acids playing an instrumental role in regulating the interaction between the gut and the brain, known as the gut-brain axis.
Short-chain fatty acids are one of the main byproducts of the microbiome and may have neuroactive properties.
Animal studies found short-chain fatty acids protecting the brain against vascular dementia and cognitive impairment. Recent results support a strong connection between nutrition, microbiome composition, and cognitive function.



 St. Petersburg, Florida
St. Petersburg, Florida
