
by admin | Sep 17, 2018 | Alzheimer’s Disease, Health Awareness, Studies
For years, medical experts have warned of the medical concerns associated with opioids, including depression, weakened immune system, and digestive issues. Now, however, new research shows that they could be particularly dangerous for dementia patients.
The Dangers of Painkillers for Dementia Patients
According to research presented at the Alzheimer’s Association International Conference, opioid-based painkillers can triple the side effects of dementia. Individuals taking the drugs experienced more pronounced personality changes, significant increases in confusion and sedation, and lower activity levels throughout the day.
In another study, researchers focused exclusively on known as “Z drugs,” which are currently given to hundreds of thousands of patients with dementia to promote sleep. Drugs under this category included zolpidem, zopiclone, and zaleplon. Findings revealed that patients on these drugs faced an increased risk of bone fracture, which contributes to an increased risk of death in people with dementia.
A Widespread Problem
Alzheimer’s, which is the most common form of dementia, currently affects an estimated 5.7 million Americans. Roughly half of the people living in care homes and suffering from this or another form of dementia experience pain to some degree, which can result from unrelated medical conditions such as arthritis. Unfortunately, as dementia patients face compounding communication challenges, treating their pain can become more difficult.
The study has prompted experts to explore other, non-pharmaceutical means of treating pain and sleep disorders in dementia patients. Alzheimer’s research group leaders believe that the solution lies in finding nondrug interventions to help manage pain and promote quality of life while minimizing serious side effects like those revealed by the study findings. Regenerative therapy may be an option to consider for those battling Alzheimer’s disease or dementia.

by admin | Sep 13, 2018 | Stem Cell Research, Stem Cell Therapy, Studies
Patients usually recover from bone fractures with the right treatment, but sometimes the bone fails to heal because new tissue does not form and connect the broken pieces properly. Delayed union refers to cases where the bone takes longer than usual to heal, and nonunion refers to cases where the bone does not heal. In approximately 5 to 10 percent of cases of a fractured bone, delayed union or nonunion occurs. These conditions are associated with long-term pain and discomfort, and though can be addressed through surgical treatments, these interventions do not always lead to long-term healing.
In recent years, researchers have begun exploring the potential for mesenchymal stem cells to help address these important challenges of delayed union and nonunion. A review of the potential for these stem cells to help in these cases where fractures do not properly heal was recently published in the Journal of Biomedical Materials Research.
Mesenchymal stem cells are helpful in bone healing because they differentiate well and can differentiate into different cell lineages that are all important for bone formation, growth, and maintenance. These cell types include chondrocytes, osteoblasts, myoblasts, and adipocytes.
According to the authors of the review, mesenchymal stem cells can be used in conjunction with extracellular matrix scaffolds and biological adjuvants that promote growth, differentiation, and blood vessel formation, to help in the bone healing process when the delayed union or nonunion occurs. Future research will help to determine the best ways that mesenchymal stem cells can be used in combination with bioengineering strategies to help patients whose bone fractures do not heal or do not heal properly.

by admin | Sep 10, 2018 | Health Awareness
Many chronic conditions, including arthritis, are characterized by chronic inflammation. While inflammation is the body’s natural immune response to healing damage, chronic inflammation takes place even when there is no injury present. It plays a role in a host of diseases, including life-threatening conditions such as heart disease and diabetes.
Researchers suspect chronic inflammation is caused by a combination of contributing factors, including family history and diet. Interestingly, recent findings are suggesting that just as certain agents may promote an inflammatory response, others may also help to block it.
Krill oil, in particular, is one dietary source which may have the ability to neutralize pro-inflammatory activity. The oil is rich in omega-3, a natural compound with anti-inflammatory properties. While other types of fish oil share similar properties, krill oil, in particular, appears to have a greater potential to promote lipid catabolism, a process involved in the breaking down of fat. Because there is a known interplay between lipid catabolism and inflammation, krill oil’s ability to stimulate the process better than other supplements is noteworthy.
Research has shown that krill oil can reduce arthritis pain and intestinal inflammation. Individuals suffering from arthritic pain saw a reduction of inflammation after one month of taking 300 mg of krill oil daily. When taken in combination with hyaluronic acid and astaxanthin, additional anti-inflammatory compounds, arthritis sufferers reported pain levels were reduced by half within three months, and 63% of study participants reported being entirely pain-free.
If you think krill oil supplements could help to alleviate your arthritis pain or minimize inflammation from another chronic condition, speak to your physician. As with any vitamins, it’s a good idea to seek input from medical professionals before taking krill oil or other anti-inflammatory supplements to assess possible interactions and receive guidance on recommended dosages.

by admin | Sep 7, 2018 | Stem Cell Therapy
Multipotent stem cells have the ability to turn into a number of different cells in the body, making them one of the most versatile solutions in regenerative medicine. They are also characterized by their capacity for self-renewal. Here, we take a look at their current applications, as well as their benefits.
What Makes Multipotent Stem Cells Unique?
To understand the distinguishing features of multipotent stem cells, we must first look at the different types of stem cells. There are three main classifications for the varying degrees of stem cell flexibility:
- Totipotent: These cells can turn into any cell in the body and are only found within the first couple of cell divisions following the fertilization of a female egg by a male sperm.
- Pluripotent: During embryonic development, totipotent cells specialize into pluripotent cells. They can give rise to all cells in the human body but aren’t quite as flexible as totipotent cells.
- Multipotent: Finally, pluripotent stem cells specialize into multipotent stem cells, which have been found in cord blood, cord tissue, adipose tissue, cardiac cells, bone marrow, and mesenchymal stem cells (MSCs).
What Are Multipotent Stem Cells Used for?
Not only are multipotent stem cells able to renew themselves almost indefinitely, their ability to become any other cell makes them a powerful agent in treating patients with tissue damage. From knees to other joints and even the gastrointestinal tract, there are many sites in the body where compromised tissue can benefit tremendously from stem cells. They can even help arthritis sufferers and individuals with tendonitis. Because stem cells can also replenish dying or damaged tissue of specialized cell types, multipotent stem cells can also benefit individuals with chronic illnesses such as COPD, multiple sclerosis (MS), and Parkinson’s disease.
What Are the Benefits of Multipotent Stem Cells?
Multipotent stem cells are advantageous because they can be sourced from a number of locations, including the Wharton’s Jelly which lines umbilical cord vessels, as well as fat tissue (adipose stem cells) and bone marrow aspirate. These cells can then be delivered via non-invasive regenerative therapy to replace damaged cells with new ones, which have the ability to help increase energy and control symptoms in chronic conditions. The treatment can also potentially spur healthy tissue development in musculoskeletal injuries, and when injected directly into the joint, it has the potential to promote healing of ligaments, tendons, and cartilage to help return functionality and in some cases could delay the need for joint replacement.

by admin | Sep 5, 2018 | Hyperbaric Oxygen Therapy, Stem Cell Research, Stem Cell Therapy, Studies, Traumatic Brain Injury
Traumatic brain injury (TBI) is one of the most common causes of disability in the United States, affecting over 13 million citizens. Traumatic brain injury is responsible for over 2 million emergency department visits, over a quarter of 1 million hospitalizations, and nearly 60,000 deaths each year.
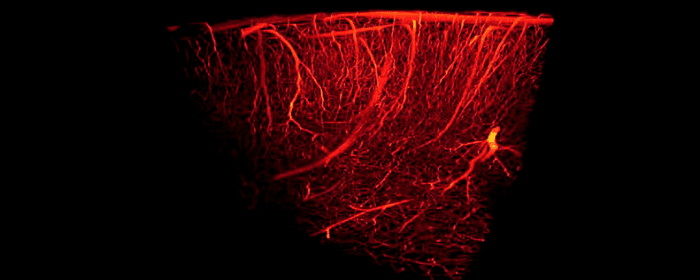
Traumatic brain injury harms brain tissue in two phases. The first phase of injury occurs at the time of the traumatic incident. This initial injury may cause small or large areas of the brain to bleed. It may also shear (stretch/tear) nerve cells, making them dysfunctional. The second phase occurs hours or days after the initial injury. The brain is subjected to ongoing damage because of inflammation, cell death, and injury to blood vessels. Many people with TBI are left with lifelong problems with thinking, memory, and behavior.
In both of these phases of injury, one major way to help prevent long-term brain damage is by maintaining adequate blood flow to brain tissue. Unfortunately, once the damage has occurred, it can be a challenge to reverse the damage. Patients usually must endure months or years of physical and occupational therapy to regain what was lost. Moreover, patients often need substantial amounts of psychiatric and psychological support to treat mental health problems.
Fortunately, researchers are using hyperbaric oxygen therapy (HBOT) to improve blood flow to the brain in patients with traumatic brain injury. Hyperbaric oxygen therapy provides patients with pure oxygen (100%) at slightly higher pressures than they would experience normally. It is been used for hundreds of years to treat scuba divers who suffered “the bends” or decompression sickness; however, researchers are finding that hyperbaric oxygen therapy is a “coveted neurotherapeutic method for brain repair.”
To study the effects of hyperbaric oxygen therapy, researchers selected 10 people who had suffered mild traumatic brain injury in the previous 7 to 13 years. Patients all had brain damage that interfered with attention, memory, and thinking abilities.
Even though patients had sustained traumatic brain injury and brain damage a decade earlier, hyperbaric oxygen therapy was able to improve blood flow in the brain. Likewise, the amount of blood detected within the brain significantly increased, suggesting that hyperbaric oxygen therapy actually caused blood vessels in the brain to grow and multiply. Just as impressively, patients with chronic brain damage performed better on tests of cognition (i.e. thinking). They were able to process information more quickly, they had better motor function, and they were able to take in and process information about the world around them more efficiently.
Because people with traumatic brain damage have limited treatment options to improve their situations, these results are incredibly exciting. This was a study on 10 patients and more studies on larger numbers are still needed to build on these findings. Nonetheless, these results are quite encouraging for people with traumatic brain injury and their loved ones.




 St. Petersburg, Florida
St. Petersburg, Florida
