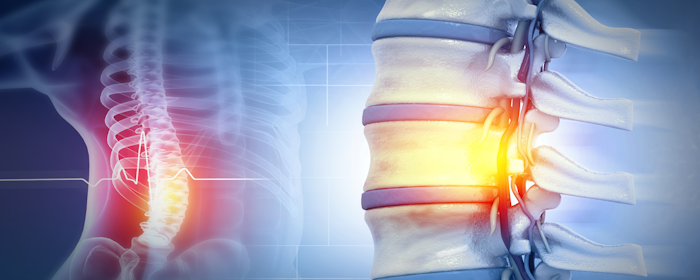
Spinal Cord Injury and the Promise of Stem Cell Therapy
Spinal cord injury (SCI) is a life-changing condition that affects hundreds of thousands of people in the United States. Each year, approximately 17,000 new cases are reported, and more than 290,000 individuals are living with long-term effects. Damage to the spinal cord can lead to partial or complete loss of movement and sensation below the…