
by admin | May 22, 2019 | Bone Marrow, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Umbilical Stem Cell
Mesenchymal stem cells have two unique and powerful properties that make them the focus of intense scientific research. First, mesenchymal stem cells can escape recognition by the immune system. In other words, when mesenchymal stem cells are infused into the body, the immune system does not recognize them as foreign and does not react to them. If the immune system did respond to the stem cells, it would cause an aggressive and potentially deadly allergic or immunologic response. Second, mesenchymal stem cells have the power to inhibit the immune system. This means mesenchymal stem cells could be used to treat immunological and autoimmune diseases such as Rheumatoid Arthritis, Systemic Lupus Erythematosus, Multiple Sclerosis, and Crohn’s Disease, among others. In essence, mesenchymal stem cells can affect the immune system without triggering an inflammatory response making them an ideal treatment for these diseases.
For some time, mesenchymal stem cells extracted from bone marrow were thought to be the only type of mesenchymal stem cells capable of beneficially affecting the immune system. This fact is not necessarily bad, but it does mean that mesenchymal stem cell donors must undergo a bone marrow procedure, which can be painful and expensive. It would be far better if doctors could use mesenchymal stem cells taken from easier-to-get tissues such as fat (adipose), umbilical cord blood, or Wharton’s jelly (umbilical cord tissue). Most people have adequate amounts of fat just under the skin, and umbilical cord blood and tissue are thrown away as medical waste every day.
Fortunately for patients, Dr. Yoo and colleagues showed that mesenchymal stem cells taken from fat tissue, umbilical cord blood, and Wharton’s jelly exhibit the same immunomodulatory properties as mesenchymal stem cells taken from bone marrow. The researchers showed that these types of mesenchymal stem cells were able to suppress T-cell proliferation as effectively as those cells taken from bone marrow. T-cell proliferation, it should be pointed out, is a key step in autoimmune inflammation that occurs in diseases such as rheumatoid arthritis and others.
In short, mesenchymal stem cells taken from easier-to-get tissues were just as effective at suppressing inflammation (in vitro) as those taken from bone marrow. These results will need to be confirmed in clinical studies; however, this approach will be much more convenient and less expensive for patients and donors if they can use mesenchymal stem cells taken from fat or umbilical cord rather than bone marrow and yet reap the same benefits.
Reference: Yoo KH et al. (2009). Comparison of immunomodulatory properties of mesenchymal stem cells derived from adult human tissues. Cell Immunology. 2009;259(2):150-6.

by admin | Sep 18, 2018 | Bone Marrow
The knee is a complex joint that must support the weight of the body while allowing the leg to bend freely. An important part of the knee joint is the meniscus. The meniscus is a fibrous cartilage structure that acts as a shock absorber. While these menisci perform very well during various strenuous activities, they can and do tear. In fact, a torn meniscus in the knee is one of the most common orthopedic injuries.
A torn meniscus of the knee often causes pain and swelling in the knee. Patients with a torn meniscus cannot squat or kneel, and the knee joint does not move smoothly. In fact, many patients with a torn meniscus describe the joint as popping, locking, catching or even “giving out.”
The meniscus of the knee can be torn in several ways; however, most torn menisci result from either one of two things: athletic activity or degenerative arthritis. As you would imagine, menisci torn during sport occur more commonly in young athletes such as dancers, certain kinds of track and field athletes, and basketball, soccer and football players. People with degenerative arthritis tend to be older and often have careers that require a lot of bending at the knee, such as carpet layers, carpenters, plumbers, etc.
Some people can live with small tears in their knee meniscus, but many people ultimately require surgery to fix the problem. One of the major approaches is to perform a total or partial meniscectomy of the damaged knee meniscus. Generally speaking, surgeons offer partial meniscectomy because patients heal faster, and results are about as good as a total meniscectomy. Unfortunately, surgical repair of these tissues is not always successful, especially in older individuals with tears related to degenerative arthritis. Consequently, surgical researchers are keen to discover new ways to improve partial meniscectomy to help people with meniscal tears of the knee.
One exciting option is using stem cells to potentially help patients regrow healthy meniscus after surgeons remove the damaged portion.
In one study, orthopedic surgeons at various surgical centers around the United States participated in an I/II, randomized, double-blind, controlled study to study the effects of human mesenchymal stem cells in people with a meniscal tear of the knee. Researchers recruited 60 patients who were eligible to receive a partial meniscectomy and sorted them into three groups: treatment group A received 50 million human mesenchymal stem cells, group B received 150 million stem cells, and group C (the control group) simply received an infusion of salt water. Patients received an injection of stem cells into the knee, 7 to 10 days after their partial meniscectomy surgery. Then researchers followed the patients for six weeks, six months, one year, and two years after the procedure.
Researchers found that some patients who received human mesenchymal stem cells had a significant increase in the size of their menisci after surgery. By contrast, no single patient in the control group had an increase in the size of their menisci. In other words, stem cells were found to be able to increase the size of the knee meniscus in some patients, as originally hypothesized. Likewise, the study authors could find no clinically important safety issues from injecting stem cells into the knees of patients. Perhaps most importantly, people who received mesenchymal stem cells reported a significant reduction in the amount of pain they experienced due to degenerative changes in the knee. In other words, partial meniscectomy plus stem cells apparently helped patients with degenerative arthritis of the knee.
The authors concluded that this research shows that human mesenchymal stem cells have the potential to be able to repair knee meniscus tissue and improve knee pain in people with meniscal tears. While additional research is needed, these results are very exciting for people who have torn menisci, especially older patients whose knee pain is a result of osteoarthritis or degenerative joint disease in the knee.

by admin | Aug 16, 2018 | Hyperbaric Oxygen Therapy, Bone Marrow, Stem Cell Research
Stem cells are generating so much excitement in research and clinical circles because they have the capacity to become many other types of cells. They also release a number of important molecules such as hormones, cytokines, and genetic material that can potentially be helpful for patients. Researchers have found that not only does hyperbaric oxygen therapy (HBOT) help in the circulation of stem cells but it also will help to mobilize stem cells from the bone marrow to the bloodstream further preparing the patient for stem cell therapy.
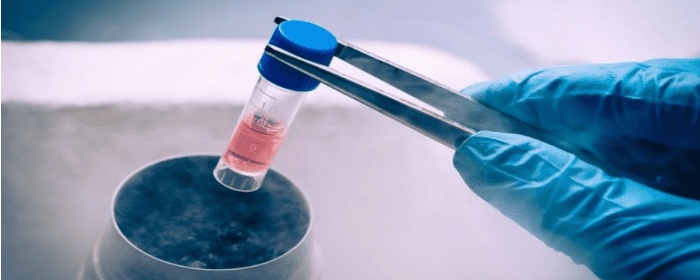
Bone marrow is a rich source of stem cells, but getting them usually requires an invasive procedure, i.e., placing a large bore needle into the middle of bone(s). Researchers have discovered, however, that hyperbaric oxygen treatment causes stem cells from the bone marrow to move into the bloodstream by specifically stimulating the body’s nitric oxide synthesis. Thus, instead of using a needle to extract stem cells from the bone marrow, patients can potentially increase their own bone marrow stem cells by undergoing hyperbaric oxygen treatment.
Stephen Thom, MD, Ph.D. and co-researchers at the University of Pennsylvania showed that a single hyperbaric oxygen treatment could double the number of bone marrow stem cells in the blood. This means that the hyperbaric oxygen was “mobilizing” the stem cells to move from the bone marrow into the bloodstream to allow them to move into areas of the body that benefit from them. Moreover, when study subjects underwent 20 treatments of hyperbaric oxygen therapy over a few weeks, the number of bone marrow stem cells in the blood increased significantly by eightfold. This astonishing finding has been confirmed in subsequent experiments.
The most important conclusion from this research is that hyperbaric oxygen therapy treatments can unlock the potential of a person’s own bone marrow stem cells without an invasive procedure. While many scientists assumed that the benefits of hyperbaric oxygen therapy were due to the high concentrations of oxygen infusing the blood, tissues, and cells, they now have research to support that these benefits may also be due to stem cell mobilization.

by admin | Aug 14, 2018 | Bone Marrow, Stem Cell Research
Colitis is inflammation of the colon, also known as the large intestine. Several things can cause colitis such as infection, medication, ischemia, or chronic inflammatory bowel disease. Inflammatory bowel diseases that affect the colon, such as ulcerative colitis or Crohn’s disease, are particularly challenging for patients. It is a chronic disease that causes cramping pain, bloody diarrhea, weight loss, fatigue, and many other chronic, challenging symptoms.
Since ulcerative colitis does not occur naturally in animals, researchers sometimes use an experimental form of colitis to mimic the disease seen in humans. This experimental colitis serves as a model to investigate treatments for inflammatory bowel disease. Essentially, researchers create a situation in which mice develop a condition that looks very much like ulcerative colitis. They develop inflammation in the large intestine, along with signs of oxidative stress and cell death. Conversely, treatments for ulcerative colitis reduce or prevent inflammation, oxidative stress, and cell death in the colon of these experimental mice.
Researchers used this model of experimental colitis to study the effect of bone marrow stem cells as a treatment for colitis. More specifically, they tested the effects of a certain part of bone marrow stem cells called extracellular vesicles. Extracellular vesicles are small spheres that containing various beneficial substances. Stem cells release these vesicles into the body. A single stem cell can release hundreds of extracellular vesicles. In fact, it is the extracellular vesicles that are believed to contain many of the useful substances that are released by bone marrow stem cells such as proteins, lipids, and nucleic acids. These substances can precisely target sick and damaged cells in the body and repair them.
Impressively, when researchers used extracellular vesicles derived from bone marrow stem cells to treat animals with experimental colitis, they observed rather extraordinary results. These vesicles protected the intestines from colitis damage. Untreated animals had severely damaged intestines when viewed under a microscope, but animals treated with extracellular vesicles had nearly normal looking intestines. Treatment also substantially reduced levels of cytokines related to oxidative stress, such as IL-1β. Extracellular vesicles derived from bone marrow stem cells also apparently blocked the intestinal cells’ ability to undergo cell suicide (apoptosis).
Taken together, these results strongly suggest that mesenchymal stem cells from bone marrow, specifically the extracellular vesicles contained within them, can dramatically improve experimental colitis. While more research is needed, this study suggests that these stem cell products could one day be a useful treatment for inflammatory bowel diseases, such as ulcerative colitis and inflammatory bowel disease.

by admin | Aug 10, 2018 | Bone Marrow, Wharton's Jelly
Mesenchymal stem cells that come from different cell sources can look similar but behave differently. Bone marrow-derived mesenchymal stem cells tend to be the gold standard for isolating and using mesenchymal stem cells, it is not particularly easy to access these cells from the bone marrow. Because there are other, much more easily accessible mesenchymal stem cells, such as those from the umbilical cord, it is important to establish the differences between the different types of stem cells so that each can be used when most appropriate and when most advantageous.
One important difference is how to isolate the cells and how easy it is to do so. Recent work published this year in Stem Cells and Development helped to define the best way to isolate mesenchymal stem cells from the Wharton’s jelly of umbilical cords. The researchers also looked at the gene expression profile and the immune system characteristics of both bone marrow-derived mesenchymal stem cells and Wharton’s jelly-derived mesenchymal stem cells.
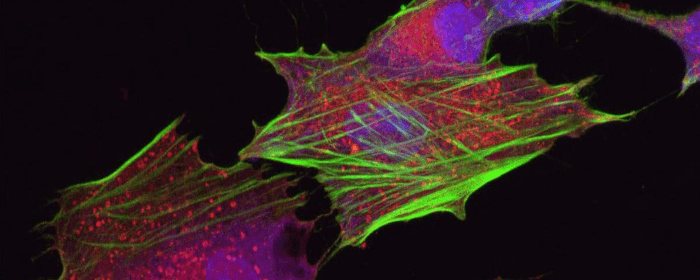
The researchers found that mesenchymal stem cells that came from the Wharton’s jelly of the umbilical cord had a better capacity to expand into more tissue than those taken from the bone marrow. Further, their gene expression was different. In the stem cells from the Wharton’s jelly, there was greater gene enrichment for genes related to cell adhesion, proliferation, and immune system functioning than in the cells from the bone marrow. These cells also induced the maturation of brain cells more so than did the mesenchymal stem cell derived from bone marrow.
These results show that Wharton’s jelly-derived mesenchymal stem cells have distinct properties from bone marrow-derived mesenchymal stem cells and likely have specific advantages as well to help treat those battling osteoarthritis, multiple sclerosis, Parkinson’s disease, and other degenerative conditions. Further research will help bear out more of the differences between these types of stem cells and how each type can best be used to help patients.

by admin | Jul 25, 2018 | Bone Marrow, Health Awareness, Stem Cell Research, Stem Cell Therapy
Stem cells derived from bone marrow, or hematopoietic stem cells, are a topic of significant debate in the medical community. While they have exhibited significant potential for benefiting people with both cancerous and noncancerous diseases including immune deficiencies, not all methods for administering bone marrow are created equal. While intra-articular injections of bone marrow are more common and considered safer, intravenous methods pose serious risks, which are explored here.
Intra-articular injections involve injecting bone marrow directly into the compromised joint, whereas intravenous methods entail infusing bone marrow stem cells into the body through the veins. Intra-articular injections have shown promise in treating conditions such as osteoarthritis (OA) in joints such as the knee and has proven to achieve pain relief for moderate-to-severe cases of osteoarthritis.
Intra-articular treatments are localized, so the injected bone marrow is already in its target location upon being administered. According to research, this form of therapy is generally considered to be safe. In intravenous bone marrow transplants, however, there are serious risks associated with treatment. Bacterial infections are common, while viral and fungal infections can also occur and cause life-threatening conditions, such as organ failure.
Risk factors for developing any complication associated with intravenous bone marrow transplantations vary based on a number of factors, including the patient’s age, genetics, and type of disease being treated. With that said, due to its limited risks, intra-articular bone marrow methods appear to be the safest form of treatment currently available. Although each patient will need to discuss risk factors alongside potential benefits with his or her physician, oftentimes the risks appear to outweigh the potential benefits.
There are alternative therapies with fewer potential side effects which may be explored such as Adipose and Umbilical Cord-derived stem cells. These regenerative medicine treatments not only can treat osteoarthritis and sports-related injury conditions, but have also shown positive results in treating neurological conditions such as Multiple Sclerosis, Parkinson’s disease, Post-Stroke, and Traumatic Brain Injuries (TBI).



 St. Petersburg, Florida
St. Petersburg, Florida
