
by admin | May 3, 2019 | ALS, Mesenchymal Stem Cells, Stem Cell Therapy
Amyotrophic lateral sclerosis or ALS is a neurological disease that causes muscle weakness, profound disability, and ultimately death. ALS is sometimes referred to as Lou Gehrig’s disease, named for the New York Yankee baseball player who developed the condition later in his life. Notably, physicist Stephen Hawking long suffered from the condition.
ALS affects the nerves that control movement. As nerve cells become dysfunctional and die, a person’s muscles become weak. The disease often starts with weakness in one part of the body before moving to other parts. In 4 out of 5 people with ALS, the first symptom is a weakness of one limb but not the other. Over time, however, the disease spreads to virtually all motor neurons (nerve cells) in the body. Eventually, patients are unable to walk because of muscle weakness and are usually confined to a wheelchair. The condition becomes particularly difficult to manage and potentially life-threatening when it starts to affect lung muscles, which make it hard for patients with ALS to breathe.
There is no cure for amyotrophic lateral sclerosis. For the most part, however, treatment for ALS focuses on reducing the symptoms of the condition rather than treating it. Patients often undergo intensive physical, occupational, and speech therapy regimens to help manage symptoms of ALS. Physicians may prescribe drugs to reduce muscle spasms, sleep problems, and pain associated with the condition. Researchers are constantly looking for ways to improve ALS treatment.
Dr. Petrou and co-authors recently reported clinical trial results in the highly regarded medical journal, JAMA Neurology. The researchers started their research by altering mesenchymal stem cells in the laboratory so that they produce neurotrophic growth factors. In other words, they engineered stem cells to release substances that help nerve cells grow and survive. Then they tested these stem cells in two clinical trials. In the first clinical trial, the doctors used these stem cells to treat six patients with early-stage ALS and six patients with advanced ALS. In the second clinical trial, they tested the stem cells in 14 patients with early-stage ALS.
All patients in both trials tolerated the stem cell treatments very well. There were no serious side effects related to treatment. 87% of the patients responded positively to treatment, which means they showed at least 25% improvement in physical function and/or lung function. These positive results from stem cell treatment are particularly impressive because ALS gets worse over time. Patients generally either stay the same or get worse—it is quite unusual for them to get better. Encouraged by these results, the researchers who worked on this study will now confirm these results in larger clinical trials. The hope is that this stem cell treatment will be available for patients with ALS in the coming years.
Reference: Petrou P. et al. (2016).Safety and Clinical Effects of Mesenchymal Stem Cells Secreting Neurotrophic Factor Transplantation in Patients With Amyotrophic Lateral Sclerosis: Results of Phase 1/2 and 2a Clinical Trials. JAMA Neurology.2016 Mar;73(3):337-44.

by admin | Apr 30, 2019 | Hyperbaric Oxygen Therapy, Stem Cell Research, Stem Cell Therapy, Traumatic Brain Injury
Traumatic brain injury (TBI) encompasses a wide range of injuries, neurological problems, and outcomes. On one end of the spectrum is a concussion, which can be mild and short lasting. At the other end of the spectrum, traumatic brain injury can be lethal or leave patients with chronic mental and physical problems. Despite this range of severities, traumatic brain injury is one of the leading causes of disability in the United States, affecting over 13 million people. People who suffer from chronic symptoms related to traumatic brain injury may struggle with chronic seizures, memory problems, concentration problems, agitation, among others. TBI can have profoundly worsened a person’s quality of life and overall well-being.
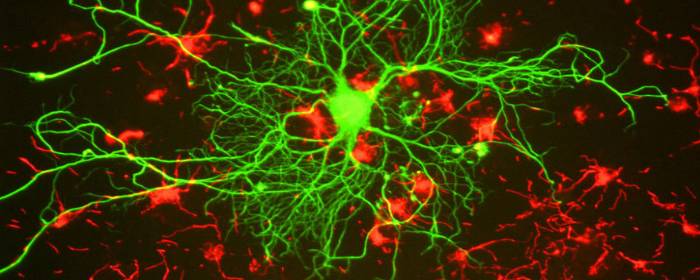
Unfortunately, little can be done to treat traumatic brain injury directly. Aside from treating symptoms, the main treatment for TBI is to have the patient to rest and avoid stimulation in an effort to give the brain time to heal. Patients can regain some function through intensive work with physical, occupational, speech, and recreational therapist. However, the brain’s ability to heal itself is limited compared to other tissues of the body. In short, the brain has very little capacity to make new brain cells after we are born. So once TBI has occurred, patients either need to depend on other healthy areas of the brain or simply adapt to their circumstances.
Fortunately, researchers are finding ways to improve on nature through hyperbaric oxygen therapy. Drs. Shandley, Wolf and other hyperbaric medicine researchers recruited a group of 28 military veterans who sustained a traumatic brain injury in Iraq or Afghanistan. These individuals had ongoing cognitive problems as a result of their brain injuries. Researchers placed some study participants in 2.4 atm avoid hundred percent oxygen, while the others simply underwent a placebo experience at basically normal pressure and oxygen levels. The two groups underwent 30 exposures each and took a cognitive test before and after these treatments.
Hyperbaric oxygen therapy increased the number of stem cells in the blood of patients with TBI. In other words, hyperbaric oxygen treatment was able to move stem cells from the bone marrow and perhaps other tissues into the bloodstream. At the same time, those treated with hyperbaric oxygen performed better on tests of cognition including ImPACT, BrainCheckers, and PCL-M test. Moreover, no adverse effects of treatment were observed. Taken together, these results suggest 30 sessions of hyperbaric oxygen treatment at 2.4 atm was able to increase stem cells in the blood and improve cognition in US warfighters who suffered traumatic brain injury during combat. These results are encouraging news for the millions of veterans and nonveterans who sustained a traumatic brain injury every year.
Reference: Shandley, S. et al. (2017). Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy. Undersea & Hyperbaric Medical Society. 2017 May-Jun;44(3):257-269.

by admin | Mar 22, 2019 | Stem Cell Research, Cannabinoid, Stem Cell Therapy
Over 1 million patients worldwide have been treated with adult stem cells and have benefited from them. And nearly 20 000 adult stem cell transplants were performed in the United States in 2014 alone! How is that possible? What are stem cells? What do they do to your body? And why are so many benefiting from them? We take a look at these important questions surrounding the benefits of stem cells, as well as how CBD can help you get the most benefits from stem cells.
What Are Stem Cells?
Stem cells are a very special kind of human cells. They are cells of the body and are therefore somatic cells, found in your bone marrow and fat cells. They are a part of your body’s natural repair process. But why are they so special? Well, they have the ability to develop into many different cell types. This can range from anything from muscle, cartilage and even bone! Stem cells can divide and become differentiated, and are therefore used as a therapy called stem cell therapy. Stem cell therapy involves using a patient’s own stem cells to repair damaged tissues. When an organism grows, the stem cells specialize and take on specific functions, including skin, nerves, blood, muscle, and liver.
Because of their magical transformative powers, they have the potential to treat a number of diseases, including diabetes, Parkinson’s and even cancer. They also have the potential to treat a number of serious injuries, from a damaged knee, to even treating spinal cord injury! Eventually, they may even be used to regenerate entire organs, decreasing the need for organ transplants. Now that we know what stem cells are and how they work, let’s have a look at five of their biggest benefits.
1. Avoid Invasive Surgery and Related Risks
One of the biggest benefits of stem cells and using them in stem cell therapy is that it allows patients who would possibly have required heavy surgery to not have any such invasive surgery. Stem cell therapy uses material already in the patient’s body, which makes it minimally invasive and also cuts out the need for an overly stressful, invasive surgical procedure. Most stem cell therapy is performed as an outpatient procedure, i.e. you can just have it done in the doctor’s office! No need for an overnight hospital stay and those ridiculously high associated medical costs.
Your doctor will first conduct a bone marrow aspiration, in which he removes stem cells from an area of the body, such as the hipbone, through a long needle. These cells are then delivered to the area of injury. Once there they work their magic to create healthy new tissue to replace a damaged muscle, tendon, ligament, cartilage or bone. They become healthy new cells that your body desperately needs.
2. Minimal Procedure & Recovery Time
One of the greatest stem cell benefits is the minimal amount of time involved in the whole therapy, from the actual procedure to the recovery time required afterward. Procedures generally last from two to five hours, depending on the type of cell treatment being performed. After the minor procedure, your activity level may be a bit limited for the first week. This is merely to let the stem cell therapy process to work uninterrupted and without any possible inflammation. After just seven days you should be able to return to your normal activity! Your treatment will include some monitoring after the treatment, to ensure everything is working as it should.
3. Can Offer Pain Relief
Stem cell therapy is highly sought out by patients who experience chronic pain. As it should be! Because of stem cells’ ability to restore and regenerate, being used in pain management is a logical step. The use of stem cell therapy is being studied for a number of chronic pain conditions, particularly pain in the knees, hips, elbows, and back. Stem cell therapy can offer pain relief in the way that it reduces the inflammation which causes chronic pain. It also helps to heal regenerative conditions that lead to pain, such as arthritis. Promising results have been found in research into the use of stem cells to reduce arthritis pain. As every patient and their condition is different, long-lasting pain relief can never be guaranteed by any doctor.
4. No Risk of Rejection
When you receive stem cells from a donor, there’s always the risk that your body will reject them. Because the stems are coming from another person’s body, many complications can arise. The most common complication is called graft-versus-host disease. This is when blood cells formed from the donor’s stem cells believe your own cells are foreign and attack them. On the other hand, harvesting stem cells extracted from your own body to generate new cells and tissues means there is no risk of rejection!
5. Potential to Discover New Treatments
Because of the nature of stem cells, the possibilities for treating new diseases and finding new cures is endless. Stem cell therapy research provides great potential for discovering treatments and cures to a variety of diseases. Advanced research is going as far as limbs and organs being grown in a lab from stem cells, which are then used in transplants. With stem cells, scientists are able to test millions of potential drugs and medicine, without the use of animal or human testers.
How Can CBD Help with Stem Cell Treatment?
We’ve seen how amazing stem cells are. Now let’s have a look at how much more amazing they can be when combined with the effects of CBD! According to results from multiple trials, cannabidiol, or CBD, can help increase the number of stem cells growing within the body. CBD has even shown to positively contribute to the movement of the stem cells within the body. They can then do what they do best – help heal the body and reduce pain.
Nearly 20% of those who went through hematopoietic stem cell transplant (HSCT) used cannabis. Not only was it used to treat their physical and emotional pain, but it was also used in the hope that it will contribute to the replacement of bone marrow that has been destroyed by cancer. Because both CBD and stem cells have been seen to reduce pain, combined the possibilities for better treatments are endless.
How Can I Experience the Benefits of Stem Cells?
You’ve heard about the many benefits of stem cells. You’ve heard how popular it is. And you’ve heard the vast amount of injuries, diseases, and pain that it can treat. Perhaps it’s about time you had a look at it as a treatment for your condition. Whether you’re looking for an alternative treatment to your sports injury, your multiple sclerosis or your chronic fatigue syndrome, we’re here to help you along the way.
Get in touch with us to see if you are a candidate for Stem Cell Therapy. Also, check out our website shop to see available products.

by admin | Jan 14, 2019 | Stem Cell Research, Stem Cell Therapy, Stroke
Patients who suffer ischemic stroke have some treatment
options, but many of them require immediate intervention and so are not useful
if too much time has elapsed between the stroke and treatment. Therapies that
employ stem cells are promising alternatives because stem cells can differentiate
into brain cells and potentially help to replace tissue that has been damaged
or destroyed.
A recent study published in Stem Cells
and Development has shown for the first time that a specific type of stem
cell – called ischemia-induced multipotent stem cells – may be able to help
with such repair of brain tissue in patients who have suffered a stroke.
Specifically, the research team demonstrated the technical ability to isolate
the ischemia-induced multipotent stem cells from the brains of elderly stroke
patients.
The scientists then used protein
binding techniques to determine where in the brain these stem cells came from.
They found that the cells came from areas of the brain where brain cells had been
damaged or killed from the stroke. These cells were located near blood vessels
and expressed certain biological markers that enabled the researchers to
confirm that they qualified as stem cells. Specifically, these cells had
proliferative qualities that suggested that they could potentially be used to
re-populate damaged areas of the brain. The cells also showed the ability to
differentiate into different types of cells, a key characteristic of stem cells
used for therapeutic purposes.
This study represents a
significant step in overcoming the technical challenges associated with
isolating and classifying ischemia-induced multipotent stem cells. The next
step for researchers will be to test the potential of these cells in stroke
treatment. If researchers show that these stem cells can be used to
successfully repair damaged areas of the brain – and more importantly, restore
functions that were disrupted by the stroke – then physicians and scientists
may be able to work together to translate these findings into therapies that
are regularly used in stroke.
Reference
Tatebayashi et al. 2017. Identification of multipotent stem
cells in human brain tissue following stroke. Stem Cells and Development, 26(11), 787-797.

by admin | Jan 4, 2019 | Stem Cell Research, Stem Cell Therapy, Studies
Spinal cord injury can be one of the most devastating
injuries. Long neurons that extend from the brain down the spinal cord are
severed and scarred. In most cases, this damage can never be repaired. If
patients survive an injury to the spinal cord, they can be permanently
paralyzed. Researchers have attempted to use high-dose steroids and surgery to
preserve the spinal cord, but these approaches are either controversial or
largely ineffective.
Ideally, one would create an environment in which nerve
cells in the spinal cord could regrow and take up their old tasks of sensation
and movement. One of the most promising approaches to do just this is stem cell
transplantation.
To test this concept, researchers used
stem cells derived from human placenta-derived mesenchymal
stem cell tissue (not embryonic stem cells) to form neural stem cells in
the laboratory. These neural stem cells have the ability to become neuron-like
cells, similar to those found in the spinal cord. The researchers then used
these stem cells to treat rats that had experimental spinal cord injury. The
results were impressive.
Rats treated with neural stem cells regained the partial
ability to use their hindlimbs within one week after treatment. By three weeks
after treatment, injured rats had regained substantial use of their hindlimbs.
The researchers confirmed that this improvement was due to neuron growth by
using various specialized tests (e.g. electrophysiology, histopathology). Rats
that did not receive stem cells did not regain substantial use of their
hindlimbs at any point in the study.
This work is particularly exciting because it shows that
stem cells can restore movement to animals who were paralyzed after spinal cord
injury. Moreover, the researchers used human stem cells derived from placenta,
which suggests that this effect could be useful in human spinal cord injury
patients (perhaps even more so than in rats). While additional work is needed,
these results offer hope to those who may one day develop severe spinal cord
injury.
Reference:
Zhi et al. (2014). Transplantation of placenta-derived
mesenchymal stem cell-induced neural stem cells to treat spinal cord injury.
Neural Regen Research, 9(24): 2197–2204.



 St. Petersburg, Florida
St. Petersburg, Florida
