
by admin | Dec 7, 2018 | Studies, Mesenchymal Stem Cells, Umbilical Stem Cell
Liver failure is a serious, potentially fatal condition in which large swaths of liver cells become dysfunctional and die. Liver failure is the result of several conditions including chronic alcohol consumption, exposure to drugs that are toxic to the liver (e.g. acetaminophen), autoimmune diseases, or infections such as hepatitis C. Liver failure causes several metabolic abnormalities including dangerously low levels of sodium, potassium, and phosphate in the blood. Moreover, four in 10 people with liver failure have trouble regulating their blood glucose levels, which can cause profound hypoglycemia. Since the liver detoxifies the blood, when the liver fails, patients can experience confusion from excessive amounts of ammonia and other substances in the blood. Seizures are also possible.
Short of liver transplantation, there are very few treatments for liver failure. Most treatments focus on restoring sodium, potassium, phosphate, and glucose levels in the blood, and bringing down ammonia levels. Fortunately, experiments show that human mesenchymal stem cells may be a promising treatment for liver failure.
Researchers enrolled 43 people with acute-on-chronic liver failure caused by hepatitis B infection. In this group, 24 patients were treated with mesenchymal stem cells derived from human umbilical cord and 19 patients received a saline solution. The groups received stem cells or placebo, respectively, three times every four weeks. Patients treated with mesenchymal stem cells showed better measures of liver function than those who received placebo. Livers of the patients treated with stem cells produced much more protein, albumin, and clotting factors, and were better able to process bilirubin. Importantly, no significant side effects were observed during the trial.
Given the serious nature of liver failure and the lack of effective treatments (besides liver transplant), this research is incredibly exciting. It offers hope that through further research scientists will be able to use mesenchymal stem cells to change the outcomes of people with acute-on-chronic liver failure.
Reference: https://stemcellsjournals.onlinelibrary.wiley.com/doi/abs/10.5966/sctm.2012-0034

by admin | Dec 3, 2018 | Osteoarthritis, Stem Cell Research, Studies
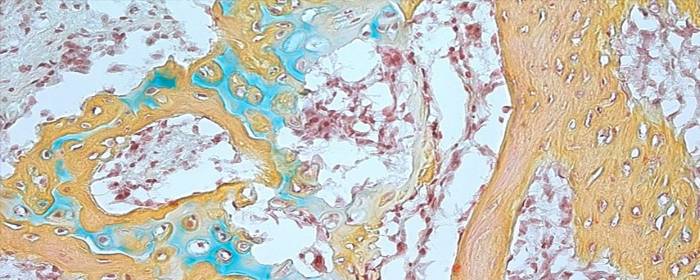
The human skeleton is made up of bone, cartilage, fat, nerves, blood vessels, and bone marrow. While the skeleton is usually strong and vibrant in youth, it changes considerably with age. Many people, especially women, experience demineralization of bone called osteoporosis. Most of us will suffer from painful, stiff, arthritic joints either from osteoarthritis or rheumatoid arthritis or both. While some of the diseases of bone and joints have specific treatments, none of them helps to restore bone and joints to their younger state. If one could reintroduce skeletal stem cells into the body, that could all change. Excitingly, researchers have recently isolated human skeletal stem cells from bone and other tissues.
At first glance, this breakthrough may not seem so surprising. One might wonder: didn’t we already have stem cells that form bone and cartilage? The answer is yes, but with an important caveat. Before researchers recently isolated human skeletal stem cells, the only stem cells that could be used to produce bone and cartilage were rather unpredictable. In addition to bone and cartilage, the mesenchymal stem cells that have been long used to form these tissues could also produce fat, muscle, fiberglass, blood vessel cells, and other tissues. In other words, the stem cells were broadly multipotent and, by extension, could not easily be used for a specific purpose, like mending bone or repairing an arthritic joint. That is why the recent discovery of these particular skeletal stem cells is so important.
The researchers isolated skeletal stem cells from various human tissues, mainly bone. They then used the skeletal stem cells to regrow bone and/or cartilage. Not only did the stem cells produce bone and cartilage in the first animal they tested, but they could retrieve stem cells from that animal and then cause bone to regrow in a second animal. This means that the skeletal stem cells have the capability of reproducing themselves.
The same researchers also discovered that when a skeleton is injured, such as in a bone fracture, the number of skeletal stem cells in that area increases dramatically. This makes sense since these cells are used to repair and regrow bone. It is also a promising result because it suggests that stem cells could be used to accelerate bone and joint healing in humans.
Scientists not directly involved in this research heralded this finding as “an extremely important advance.” However, they also acknowledge that more work needs to be done before skeletal stem cells can be routinely used in patients with orthopedic conditions. Nevertheless, these results are an exciting development in the field of stem cell research and orthopedics.
Reference: https://www.sciencenews.org/article/humans-have-skeletal-stem-cells-help-bones-and-cartilage-grow

by admin | Nov 28, 2018 | Stem Cell Therapy, Wharton's Jelly
Perinatal stem cells have been attracting attention globally in recent years due to their potential in regenerative medicine. These stem cells come in many forms, due to the wide variety of potential sources for these cells. Perinatal stem cells, for instance, may be umbilical cord-derived hematopoietic stem cells, amniotic epithelial cells, amniotic fluid stem cells, or chorionic mesenchymal stem cells. All sources, nonetheless are considered biological waste and are therefore usually discarded after delivery of babies.
Importantly, perinatal stem cells, despite their origin, tend to share a number of characteristics that make them beneficial in treating conditions. Additionally, unlike other sources of stem cells, retrieval of perinatal stem cells is noninvasive and does not require the ethical considerations that retrieval from other sources may involve. A recent review in Regenerative Medicine has highlighted the potential benefits of perinatal stem cells in therapeutic interventions.
In addition to the relatively easy collection and preparation of perinatal stem cells, these cells tend to be easily harvested and manipulated without harming either the mother or the baby. Upon collection, these stem cells exist in high volume and have greater ability to proliferate than other stem cell types such as bone marrow stem cells. Research has also shown that these cells tend not to lead to adverse immune reactions, though the mechanisms involved in their relationship to the immune system are not well understood.
Given their relative advantages over other stem cell types, perinatal stem cells are well poised to be used in cell-based therapies targeting a wide variety of conditions. Future research will help to define the precise role these cells can play in regenerative medicine and which conditions they may be most useful for.

by admin | Nov 19, 2018 | Adipose, Osteoarthritis, Stem Cell Research, Stem Cell Therapy
Bone generally develops via one of two distinct mechanisms: intramembranous ossification and endochondral ossification. In the former case, mesenchymal progenitor cells directly differentiate into osteoblasts that form bone. In the latter case, the mesenchymal progenitor cells first create a matrix of cartilage that then acts as a template to enable the remodeling or development of bone tissue. This process of endochondral ossification is the predominant way that bone is generating during the healing process after bones are broken and fractures are endured. Using stem cells to facilitate this process can, therefore, be beneficial in non-healing bone fractures.
A new study published in Acta Biomaterialia has proposed that adipose tissue can be used in bone generation as a scaffold on which adipose mesenchymal stem cells can expand and allow for endochondral ossification. The researchers showed how adipose tissue could be used in this way, through what they termed Adiscaf, to successfully generate cartilage tissue and eventually bone tissue formation. The bone tissue that formed through this process contained bone marrow elements, further demonstrating the bone’s integrity and the promise of this procedure.
Compared to other strategies for building scaffolding, this strategy appeared successful because by using adipose tissue, the adipose stem cells were exposed to their native environment and therefore likely maintained functions they otherwise may not have. Not only will these findings help to solidify our understanding of how to nurture stem cells and enable them to differentiate in ways that can be therapeutically applicable, but they also specifically show how adipose tissue may be able to be used to generate a bone organ through endochondral ossification. Future research will likely help to clarify how these findings can be applied to patients to improve bone healing.

by admin | Nov 14, 2018 | Stem Cell Research, Stem Cell Therapy
Evidence has been accumulating for years showing how stem cells can serve therapeutic functions. Much of this research focuses on how stem cells can be applied to damaged tissue to help regenerate the area. Because stem cells can differentiate into a wide variety of cell types, they can be widely utilized to repair distinct types of tissue. However, a recent paper published in the World Journal of Stem Cells has described how stem cells can also be used to carry therapeutic agents to tissues and organs to help with regeneration.
Stem cells are good candidates for delivering genes, proteins, and small molecules to areas of interest because they have an innate ability to migrate to sites of injury. One challenge for using stem cells for this type of therapeutic delivery is how to load the stem cells with the therapeutic agents. There are pros and cons for the techniques that have been investigated.
Polymeric nanoparticles, are FDA approved and are versatile, uploaded efficiently, and biocompatible. However, it is hard to control the release of the therapeutic agent from the stem cells. Magnetic nanoparticles are not associated with high levels of toxicity and are efficient with loading. However, they can induce oxidative stress in carrier cells.
Silica nanoparticles have quick uptake, are non-toxic, stay within cells for a long time, and are versatile. However, their tendency to stay within cells for a long time can sometimes be a disadvantage when the agent needs to be cleared.
Liposomal nanoparticles are relatively easy to manufacture and are versatile in their therapeutic agent delivery. However, these nanoparticles are less efficient at uptake and need higher concentrations of the therapeutic agent loaded, which can be toxic to cells.
Once stem cells are loaded with bioactive molecules, there are a few ways that they can be guided toward target organs. For instance, they can be systemically infused so that they can migrate to their target areas trough blood flow.
Further research will help to clarify how well stem cells can be used to help deliver therapeutic agents to damaged or impaired tissue. Investigation into the different nanoparticles, stem cells, and potential therapeutic applications will help us better understand the extent to which stem cells can be used in regenerative medicine.


 St. Petersburg, Florida
St. Petersburg, Florida
