
by admin | May 3, 2019 | ALS, Mesenchymal Stem Cells, Stem Cell Therapy
Amyotrophic lateral sclerosis or ALS is a neurological disease that causes muscle weakness, profound disability, and ultimately death. ALS is sometimes referred to as Lou Gehrig’s disease, named for the New York Yankee baseball player who developed the condition later in his life. Notably, physicist Stephen Hawking long suffered from the condition.
ALS affects the nerves that control movement. As nerve cells become dysfunctional and die, a person’s muscles become weak. The disease often starts with weakness in one part of the body before moving to other parts. In 4 out of 5 people with ALS, the first symptom is a weakness of one limb but not the other. Over time, however, the disease spreads to virtually all motor neurons (nerve cells) in the body. Eventually, patients are unable to walk because of muscle weakness and are usually confined to a wheelchair. The condition becomes particularly difficult to manage and potentially life-threatening when it starts to affect lung muscles, which make it hard for patients with ALS to breathe.
There is no cure for amyotrophic lateral sclerosis. For the most part, however, treatment for ALS focuses on reducing the symptoms of the condition rather than treating it. Patients often undergo intensive physical, occupational, and speech therapy regimens to help manage symptoms of ALS. Physicians may prescribe drugs to reduce muscle spasms, sleep problems, and pain associated with the condition. Researchers are constantly looking for ways to improve ALS treatment.
Dr. Petrou and co-authors recently reported clinical trial results in the highly regarded medical journal, JAMA Neurology. The researchers started their research by altering mesenchymal stem cells in the laboratory so that they produce neurotrophic growth factors. In other words, they engineered stem cells to release substances that help nerve cells grow and survive. Then they tested these stem cells in two clinical trials. In the first clinical trial, the doctors used these stem cells to treat six patients with early-stage ALS and six patients with advanced ALS. In the second clinical trial, they tested the stem cells in 14 patients with early-stage ALS.
All patients in both trials tolerated the stem cell treatments very well. There were no serious side effects related to treatment. 87% of the patients responded positively to treatment, which means they showed at least 25% improvement in physical function and/or lung function. These positive results from stem cell treatment are particularly impressive because ALS gets worse over time. Patients generally either stay the same or get worse—it is quite unusual for them to get better. Encouraged by these results, the researchers who worked on this study will now confirm these results in larger clinical trials. The hope is that this stem cell treatment will be available for patients with ALS in the coming years.
Reference: Petrou P. et al. (2016).Safety and Clinical Effects of Mesenchymal Stem Cells Secreting Neurotrophic Factor Transplantation in Patients With Amyotrophic Lateral Sclerosis: Results of Phase 1/2 and 2a Clinical Trials. JAMA Neurology.2016 Mar;73(3):337-44.

by admin | Apr 19, 2019 | ALS, Mesenchymal Stem Cells, Stem Cell Research
Amyotrophic lateral sclerosis (ALS) is an incurable neurologic disorder that causes muscle weakness, and disability. In ALS, nerve cells degenerate causing muscle weakness and atrophy. ALS affects the nerve cells that connect the brain to the spinal cord (upper motor neurons), and nerve cells that connect the spinal cord to muscles (lower motor neurons). While some patients with ALS will experience paresthesias (numbness and tingling), most nerves that detect sensations remain intact until the very latest stages of the disease. Over time, people with ALS may experience cognitive problems such as mild dementia, though most stay mentally sharp. Patients with ALS may also experience Parkinson’s-like symptoms, such as tremor and slowness of movement (bradykinesia). When the nerves that control swallowing or breathing become dysfunctional, ALS can become life-threatening or lethal. Damage to these nerves and muscles could lead to aspiration pneumonia, and respiratory failure, respectively.
ALS is also known as Lou Gehrig’s disease because the famed New York Yankee publicly struggled with ALS. Perhaps people alive today are more familiar with another patient who suffered from ALS, the Nobel laureate physicist, Stephen Hawking. Dr. Hawking was well known for being confined to a wheelchair and almost completely paralyzed, requiring a specialized computer interface to communicate.
There is no specific treatment for ALS. Therapy is aimed at controlling the symptoms of the disease. For example, patients may have a breathing tube placed in their neck (tracheostomy) and be connected to a ventilator to help support breathing. Likewise, a feeding tube in the stomach can help patients receive hydration and nutrition if they cannot safely swallow food because of neck muscle weakness. Physical therapists help patients maximize the strength and function. Certain medicines can be used to help treat muscle spasms, sleep problems, pain, and depression.
Since there is no cure for ALS, and really no specific treatment for the condition, there is considerable interest in discovering effective treatments. One of the most promising potential therapies is to use stem cells to treat ALS. Since ALS is caused by the destruction and loss of motor neurons, a reasonable treatment approach is to use stem cells that can become motor neurons and promote motor neuron growth and development.
Recently, researchers conducted two clinical trials to evaluate the safety and feasibility of using bone marrow-derived mesenchymal stromal cells to treat patients with ALS. In one clinical trial, the researchers infused stem cells intravenously, while in the other they infused the stem cells into the cerebrospinal fluid around the spine (intrathecally). Patients in both trials were followed for up to 12 months after the infusion to see if the stem cells caused side effects. During the follow-up period, there were no reports of adverse events related to the treatment. Given the success of these trials, this work clears the way for future clinical trials to study the efficacy of stem cells for treating amyotrophic lateral sclerosis.
Reference: Nabavi et al. (2019). Safety, Feasibility of Intravenous and Intrathecal Injection of Autologous Bone Marrow-Derived Mesenchymal Stromal Cells in Patients with Amyotrophic Lateral Sclerosis: An Open-Label Phase I Clinical Trial. Cell Journal. 2019 Jan;20(4):592-598.

by admin | Mar 8, 2019 | Mesenchymal Stem Cells, Multiple Sclerosis, Stem Cell Research, Stem Cell Therapy
Of all conditions that affect the central nervous system, Multiple Sclerosis (MS) is the most common in young adults. The severity of multiple sclerosis varies considerably and can affect almost every organ system in the body affecting eyesight, bowel function, bladder function, and sexual function. Multiple sclerosis may cause cognitive problems, depression, seizures, fatigue, and pain. Most people with multiple sclerosis will have a relapsing-remitting course, which means they will have periods of relative health punctuated by flare-ups of the condition. About one out of ten people with the condition will have primary progressive multiple sclerosis, which means once the disease occurs it almost constantly causes symptoms and progresses over time.
Multiple sclerosis appears to be an inflammatory condition that affects the covering around nerves. During acute flareups/exacerbations, physicians usually prescribe a powerful steroid medication such as methylprednisolone to combat the inflammation. Patients with multiple sclerosis generally always require some sort of treatment to help manage their immune system. No fewer than 15 immune modulating treatments have been used to treat multiple sclerosis, none of which provides a cure. As such, researchers are seeking new and innovative ways to treat this potentially debilitating condition.
Researchers at the Tisch Multiple Sclerosis Research Center of New York chose to focus their research efforts on a particular type of stem cell, namely bone marrow-derived mesenchymal stromal cells. The researchers harvested these cells from the patients themselves (autologous stem cells). Then, in their laboratory, scientists used various means to prompt the cells to become neural progenitors. A neural progenitor cell is a cell that can become any of the three main types of brain cells: neurons, astrocytes, or oligodendrocytes. Incidentally, oligodendrocytes are believed to be most affected in multiple sclerosis.
Harris and co-authors at the Tisch Center enrolled six patients with progressive multiple sclerosis. These six patients had failed to find relief from other conventional multiple sclerosis treatments. The researchers provided between 2 to 5 infusions of neural progenitor cells into the spinal fluid. The multiple sclerosis patients treated with the cells tolerated the treatment very well. No serious adverse events occurred, nor were there any safety concerns during treatment. Impressively, four of the six patients—for whom no other multiple sclerosis treatment worked—had a measurable clinical improvement after stem cell treatment.
Based on the results of this clinical study, the scientists concluded that neural progenitor cells created from autologous mesenchymal stromal cells were safe to use in patients with primary progressive multiple sclerosis. Moreover, the beneficial effect witnessed in two-thirds of treated patients suggests that these cells may be able to help patients with even the most severe and difficult-to-treat forms of multiple sclerosis. Of course, additional testing is required before this treatment becomes commonplace, but the results of this first-in-human clinical study are extremely encouraging.
Reference: Harris et al. (2016). Clinical safety of intrathecal administration of mesenchymal stromal cell-derived neural progenitors in multiple sclerosis. Cytotherapy. 2016 Dec;18(12):1476-1482.

by admin | Mar 1, 2019 | Mesenchymal Stem Cells, Osteoarthritis, Stem Cell Therapy, Studies
Cartilage plays several important roles in the way joints move and function. Joint cartilage provides lubrication, acts as a shock absorber, and helps the joint move smoothly. Joint cartilage is comprised of two substances chondrocytes (i.e. cartilage cells) and extracellular matrix (proteins such as hyaluronic acid, collagen, fibronectin, etc.).
Many conditions can lead to joint cartilage defects. In young people, the most common cause of the joint cartilage defect is an injury. For instance, a football player suffers a hard contact that injures the joint. Another example is a gymnast who repeatedly places substantial impact forces on the knee and other joints of the lower body, resulting in damage. In older people, the most common cause of joint cartilage defects is Osteoarthritis. Over time, the joint cartilage breaks down in the cartilage loses its ability to lubricate, absorb shock, and support the smooth movement of the joint. This leads to stiffness, pain, and “trick” joints, among other symptoms.
Orthopedic surgeons, rheumatologists, and other physicians have attempted to treat these conditions by injecting the damaged joint with one of the two main components of joint cartilage: extracellular matrix. Physicians inject hyaluronic acid (and sometimes related extracellular matrix proteins) to help replace and restore damaged joints. This approach can be helpful for some patients, but it is certainly not a cure.
Only recently, have researchers attempted to replace the other component of joint cartilage: chondrocytes. Specifically, researchers have focused their efforts on mesenchymal stem cells that have the ability to differentiate and become cartilage cells. Li and colleagues injected combinations of bone marrow-derived mesenchymal stem cells and hyaluronic acid into animals with experimental cartilage defects. They showed that hyaluronic acid injections alone modestly repaired the cartilage damage. However, when stem cells plus hyaluronic acid was injected, the joints were almost completely repaired. In other words, stem cells plus hyaluronic acid resulted in much greater improvement in joint cartilage damage than hyaluronic acid alone.
The authors of the study concluded that “bone marrow stem cells plus hyaluronic acid could be a better way to repair cartilage defects.” While additional work is needed, these results are extremely exciting for people who suffer from joint cartilage defects such as osteoarthritis. In the future, people who are candidates for hyaluronic acid injection treatments may instead receive a combination of hyaluronic acid plus stem cells and may enjoy an even greater benefit than hyaluronic acid treatment alone.
Reference: Li et al. (2018). Mesenchymal Stem Cells in Combination with Hyaluronic Acid for Articular Cartilage Defects. Scientific Reports. 2018; 8: 9900.

by admin | Feb 4, 2019 | Adipose, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy
Spinal cord injury is severe neurological condition in which
the major mode of transmission between the brain and the body is disrupted.
When higher levels of the spinal cord are injured, for example, in the neck,
the injury can be immediately fatal. Those who survived spinal cord injury are
often left paralyzed and at risk for a number of comorbid conditions
such as pneumonia, depression, skin ulceration infection, urinary tract
infections, and pain.
If patients who sustain spinal cord injury can receive
medical treatment quickly, physicians may administer glucocorticoids to help
reduce swelling around the injury and preserve spinal cord function. Patients
may also undergo therapeutic
hypothermia (a.k.a. targeted temperature management, whole body cooling),
also to help reduce inflammation and prevent scar tissue from forming around
the damaged spinal cord.
After the first few days to weeks after spinal cord injury,
not much can be done to change the outcome of the disease. Patients may undergo
intensive physical, occupational, and speech therapy to help regain function,
but more often than not the neurological deficits are mostly permanent. Hence,
researchers are feverishly searching for ways to treat spinal cord injury and,
by extension, prevent or reduce paralysis and other chronic complications.
Mesenchymal stem cells are an intriguing potential therapy
for spinal cord injury. These cells can easily be obtained from many different
tissues including bone marrow and fat among others. In animals, mesenchymal stem
cells have been shown to improve changes that occur during spinal cord injury,
namely the regeneration
and strengthening of nerve cells in the spinal cord. Research
has also shown how adipose-derived stem cells are a potential option for those
with neurological conditions such as spinal cord injury.
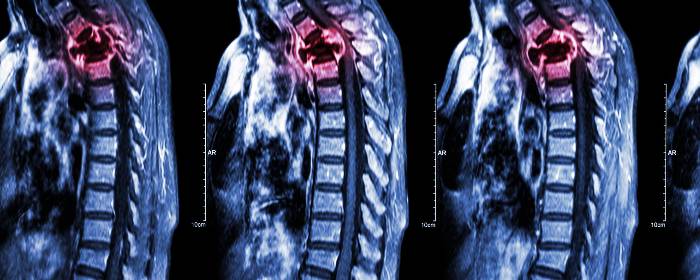
To test this possible effect in humans, researchers collected
mesenchymal stromal (stem) cells from patients with spinal cord injury in
their upper back (i.e. thoracic spinal cord). Researchers then prepared and administered
those cells back into the cerebrospinal fluid of the same patients. Each
patient received two or three injections of approximately 1,000,000 cells per
kilogram body weight. There were no adverse effects of the treatment for up to
two years after injection. MRI imaging showed no abnormalities resulting from
stem cell infusion. While the authors write that there were too few patients to
make any firm conclusions about the efficacy of the treatment, they were
strongly encouraged by the safety of the procedure. In fact, they use these
results to begin a placebo-controlled clinical trial.
Reference
Satti et al. (2016). Autologous mesenchymal stromal cell
transplantation for spinal cord injury: A Phase I pilot study. International Society for Cellular Therapy,
18(4),518-522.


 St. Petersburg, Florida
St. Petersburg, Florida
