
by admin | Jul 30, 2021 | Stem Cell Research, Multiple Sclerosis, Stem Cell Therapy
Typically understood to support hematopoiesis and to produce the cells of the mesodermal lineage, mesenchymal stem cells (MSCs) found in bone marrow, fat, and other tissues of the body, have recently been found to contain additional properties that include immunomodulator and neurotrophic effects.
Considering earlier studies that have demonstrated favorable effects of MSC treatments in a variety of conditions – including stroke, multiple sclerosis, multi-system atrophy, and amyotrophic lateral sclerosis, Petrou et al. performed this double-blind study as a way to evaluate the best way of administration and the safety and clinical efficacy of MSC transplantation – specifically in patients with active and progressive multiple sclerosis.
The response of the 48 patients with progressive multiple sclerosis and with displaying evidence of either clinical worsening or activity during the previous year in this study were evaluated after being treated intrathecally (IT) or intravenously (IV) with autologous MSCs or with sham injections. Having identified a critical and unmet need for treatment, the goal of Petrou et al.’s study was to examine the therapeutic efficacy of MSC transplantation in this specific population.
Over the course of this controlled clinical trial, participants were randomly assigned to three treatment groups and treated (either intrathecally or intravenously) with autologous MSCs or with sham injections. At the 6-month mark, the authors of this study retreated half of the patients in both the MSC-IT and MSC-IV groups with MSCs, while the remaining participants were treated with sham injections. The same process occurred with patients initially treated with sham injections; meaning that at the 6-month mark, half were either treated with MSC-IT or MSC-IV.
Prior to the start of this study, Petrou et al. established a number of primary and secondary endpoints. Predetermined primary endpoints of this study included: the safety of the MSC-IV and MSC-IT treatments and the difference among the three groups in relation to performance on the Expanded Disability Status Scale (EDSS) at 6- and 12-month intervals. Predetermined secondary endpoints included the difference between the sham-treated and MSC-IT or MSC-IV treated group in the number of relapses and the relapse rate, the number of MRI gadolinium-enhancing lesions, the annualized rate of change in the T2 lesion load on MRI, percent brain volume change, performance on a series of physical and cognitive functions, and the retinal nerve fiber layer thickness.
At the conclusion of this 14-month trial, the authors reported that the study demonstrated positive results in all predetermined primary endpoints. More specifically, throughout the course of this study, the authors discovered that significantly fewer patients experienced treatment failure in the MSC0IT and MSC-IV groups compared with those in the sham-treated group. Additionally, over the course of the following year, nearly 59% and 41% of patients treated with MSC-IT and MSC-IV exhibited no evidence of multiple sclerosis activity; this is compared with less than 10% of patients in the sham-treated group.
Significant improvements of those receiving MSC-IT treatment (compared to sham treatment) were also observed in the following: ambulation index, the sum of functional scores, 25-foot timed walk test, 9-hole peg tests, PASAT and OWAT/KAVE cognitive tests, and newer biomarkers, including retinal nerve fiber layer and motor network. The authors also report beneficial, but less significant effects were observed in the MSC-IV groups.
Although the authors report a number of limitations associated with this study, including a small number of patients in each group, the short duration of the study, and the crossover design of the study (which could have resulted in a “carry-over” effect from the first cycle of treatment), they also conclude that the clinically significant findings observed in patients with progressive multiple sclerosis who were previously unresponsive to traditional or conventional therapies provide clear evidence of short-term efficacy and possible indications of neuroprotection induced by administration of autologous MSCs in patients with progressive multiple sclerosis.
In addition, the authors found that intrathecal administration of MSCs appears more beneficial than intravenous, as well as the potential benefits provided by receiving repeated injections of MSCs.
As such, Petrou et al. conclude by calling for a larger phase III study to confirm these findings and as a way to further evaluate the therapeutic potential of autologous MSCs in neuroinflammatory and neurodegenerative diseases, including active progressive multiple sclerosis.
Source: (2020, December 1). Beneficial effects of autologous mesenchymal stem cell … – PubMed. from https://pubmed.ncbi.nlm.nih.gov/33253391/

by admin | Nov 27, 2019 | Crohn's Disease, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy
Crohn’s disease, a form of chronic inflammatory bowel disease, affects an estimated 700,000 people in the United States, affecting men and women equally. While the disease is characterized by abnormal inflammation in the gastrointestinal and digestive tracts, some people with the illness develop perianal Crohn’s disease. In this case, the inflammation extends to areas around the anus. The precise proportion of Crohn’s disease patients who develop perianal Crohn’s disease is debated, but the need for better treatments for the condition is not. A new and unique treatment is the use of stem cells to treat Perianal Crohn’s Disease.
Unfortunately, though there are several drug and surgical interventions that have been developed to treat perianal Crohn’s disease, each of the available treatment options suffers critical limitations, including risks for adverse side effects. There is no available therapeutic approach that successfully achieves long-term remission.
Based on the need for – and lack of – more efficacious interventions for perianal Crohn’s disease and the ability of cell-based therapies to address similar types of disease, researchers have positioned that stem cell therapy may be a promising avenue for the relevant patient population. A recent review published in the Journal of Crohn’s and Colitis covers the research that has been conducted to address this possibility and the data that suggest that mesenchymal stem cells could provide a safe and effective way to treat perianal Crohn’s disease without the unwanted side effects associated with conventional treatment options.
In this review, the authors cover clinical trials on cell-based therapies for perianal Crohn’s disease, including phase 1, phase 2, and phase 3 randomized controlled trials. The authors consider the differences in outcomes between conventional treatments and cell-based therapies and offer suggestions for the direction of research into the use of stem cells for the treatment of perianal Crohn’s disease.
Reference: Lightner, A.L. & Faubion, W.A. (2017). Mesenchymal stem cell injections for the treatment of perianal Crohn’s disease: What we have accomplished and what we still need to. Journal of Crohn’s and Colitis, 11(10), 1267-1276.

by admin | Nov 15, 2019 | Adipose, Heart Failure, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy
A myocardial infarction, commonly known as a heart attack, occurs when blood flow through the coronary arteries is blocked. A heart attack usually happens to people with atherosclerotic coronary heart disease, which narrows one or more of the coronary arteries. A blood clot becomes lodged in the narrowed artery, preventing blood from reaching the heart muscle. Because the heart needs a virtually constant supply of oxygen-rich blood to survive, an interruption in blood flow to the heart can quickly cause muscle cells to die. There has been much talk in the medical community of using stem cells to rebuild the heart after a heart attack.
Dead heart muscle cells cannot help the heart pump blood. Thus, people who suffer a heart attack are often left with “weak” hearts. Instead of strongly squeezing blood out of the heart to the rest of the body, a larger portion of the blood remains in the heart (i.e. reduced ejection fraction). People who have had a heart attack that reduces ejection fraction commonly develop a condition known as congestive heart failure.
People with congestive heart failure often have difficult lives. Congestive heart failure patients periodically experience exacerbations that require hospitalization. They are put on restrictive diets; their salt and fluid intakes are limited. They must also take several different medications to help the heart pump blood through the arteries to the body and keep fluid levels in the body low. These medications do not heal or replace dead heart muscle cells. Instead, they make the remaining cells work harder (or decrease resistance in the arteries, or help the body eliminate fluid through urination).
What is needed is a way to regenerate dead heart muscle cells. Fortunately, several research groups are working on ways to use stem cells to regenerate heart muscle cells so that heart attack patients can regain heart muscle function.
There have been at least 11 clinical trials studying the effects of stem cells on patients with myocardial infarction. The trials show that stem cell infusion into the vein, the coronary artery, or the heart muscle itself is safe and well-tolerated by patients. Notably among the studies, patients with acute myocardial infarction who received allogeneic human mesenchymal cells intravenously had a better ejection fraction, better heart structure, and better lung function after six months than those who received a placebo. In the APOLLO trial, patients with acute myocardial infarction who received adipose-derived mesenchymal cells had half the dead heart muscle cells than those who received a placebo (i.e. lesion volume was 50% lower in treated patients).
Phase III clinical trials are considered definitive (pivotal) evidence of benefit. In phase III C-CURE trial, patients with heart failure due to coronary artery disease received autologous mesenchymal cells (i.e. their own cells, specially prepared). Treated patients enjoyed significantly increased ejection fraction (heart-pumping ability) and better functional capacity and quality of life. Other Phase II clinical trials (ADVANCE, CONCERT-CHF, TRIDENT, POSEIDON-DCM) are ongoing.
These results are welcome news for patients who suffer—or will one day suffer—from a heart attack, an event that happens in 735,000 Americans every year.
Reference: Golpanian, S. et al. (2016). Rebuilding the Damaged Heart: Mesenchymal Stem Cells, Cell-Based Therapy, and Engineered Heart Tissue. Physiological Reviews. 2016 Jul; 96(3): 1127–1168

by admin | Nov 13, 2019 | Stem Cell Research, Exosomes, Mesenchymal Stem Cells
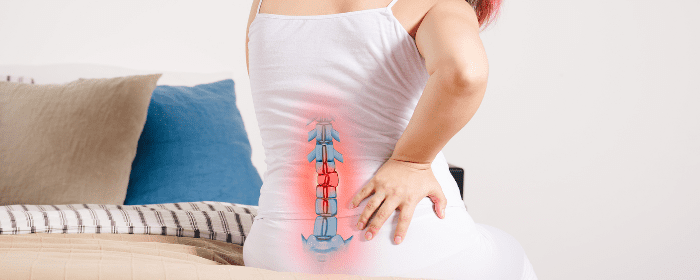
The spinal column is made up of more than a dozen vertebral bones stacked on top of each other. Since the spine is not a single bone, it is capable of pivoting and bending, which gives the torso a degree of flexibility. A key part of this structure relies on the substance between the vertebral bones called the intravertebral disc.
The intravertebral disc is made up of the annulus fibrosis (the tough outer ring) and the nucleus pulposus (the jelly-like inner core). Each intervertebral disc acts as a shock absorber between the vertebral bones. Over time and with age, however, the intervertebral disc tends to breakdown. This can cause called degenerative disc disease, which includes herniated discs (“slipped discs”), pinched nerves, neck and back pain, and nerve problems. Obviously, finding ways to reverse or prevent intravertebral discs from breaking down is of great medical and scientific interest and for the countless patients with degenerative disc disease.
As with other groups interested in regenerative medicine, researchers have turned to stem cells in an effort to regenerate tissue within the intravertebral disc. One research group reported their recent success using bone marrow-derived mesenchymal stem cells. The scientists collected exosomes—very small packets filled with highly concentrated molecules such as proteins, microRNA, transcription factors and lipids—from these stem cells. In this study, researchers also collected exosomes from nucleus pulposus cells and tested the exosomes in various ways.
The researchers found that exosomes could send out signals to bone marrow mesenchymal cells and call them to the intervertebral disc. The exosomes also prompted the stem cells to become new nucleus pulposus-like cells. Conversely, exosomes from bone marrow mesenchymal cells caused nucleus pulposus cells to grow and multiply (i.e. proliferate). Finally, exosomes helped the tissue in degenerating vertebral discs to express the same genes as healthy discs.
While these results are complex, they suggest that exosomes from bone marrow mesenchymal cells and nucleus pulposus cells work together to recruit and make more healthy cells in degenerating vertebral discs. This could have profound implications for the millions of people with degenerative disc disease. If these results are confirmed in clinical trials, it would mean that exosomes could be used to prevent or reverse degenerative disc disease. We anxiously await further work in this exciting field.
Reference: Kang L. et al. (2017). Exosomes as potential alternatives to stem cell therapy for intervertebral disc degeneration: in-vitro study on exosomes in interaction of nucleus pulposus cells and bone marrow mesenchymal stem cells. Stem Cell Research Therapy. 2017; 8: 108.

by admin | Oct 23, 2019 | Age Management, Stem Cell Research, Stem Cell Therapy
Autologous stem cell treatments offer several advantages over other forms of stem cell treatment. In autologous stem cell treatment, a patient’s own stem cells are retrieved, processed, and injected back into the patient’s body. There is no need for a stem cell donor, and the entire procedure can take place in the same medical office. Since the patient’s own cells are used for an autologous stem cell treatment, there is no risk of disease transmission from a donor (because there is no donor) and no risk of rejection (because they are the patient’s own stem cells).
Unfortunately, younger stem cells are better for regenerative medicine than older stem cells are. Moreover, older people have fewer stem cells that can be harvested than they did when they were younger. So while autologous stem cell treatment is still advantageous, it becomes more difficult to achieve as patients get older because their stem cells are fewer and less potent. Making matters worse, older stem cells compete against more youthful stem cells, making autologous stem cell treatments potentially even less effective in older patients.
Fortunately, stem cell researchers are coming up with ways to make the most out of the stem cells that older patients still have. They still take a sample of tissue, such as fat, and harvest the stem cells contained within it. However, instead of injecting all stem cells from the sample (both older and youthful stem cells), researchers select and use only youthful stem cells. Furthermore, they make the treatments even more effective by injecting other substances (e.g. extracellular matrix) that helps youthful stem cells survive, grow, and thrive.
To demonstrate the effectiveness of their approach, researchers collected mesenchymal stem cells from about a dozen older individuals aged 65 to 86 years old. They then assorted the stem cells into different groups, separating youthful from older stem cells. They then used special factors to help the youthful stem cells grow, increasing the numbers by an impressive 17,000 times. So while only 8% of stem cells produced by older individuals are “youthful,” this laboratory process increased those numbers to a point that they can be used for stem cell treatments—even stored for future use!
The next phase of the research will be to inject these youthful stem cells into older patients and assess their effectiveness. However, even these preliminary results are exciting, because they suggest that people of all ages can potentially benefit from autologous stem cell treatments, not just middle age and younger individuals.
Reference: Block, TJ et al. (2017). Restoring the quantity and quality of elderly human mesenchymal stem cells for autologous cell-based therapies. Stem Cell Research and Therapy. 2017 Oct 27;8(1):239.


 St. Petersburg, Florida
St. Petersburg, Florida
