
by admin | Mar 5, 2020 | Hair Regrowth
Androgenic alopecia, more commonly known as pattern hair loss or pattern baldness, is an extremely common form of hair loss. Four out of 5 men and 2 out of 5 women under the age of 70 have hair loss due to androgenic alopecia (aka androgenetic alopecia). While this form of hair loss is not deadly, or even dangerous, it can cause substantial amounts of personal suffering, low self-esteem, and diminished quality of life. Indeed, most people with androgenic alopecia or pattern hair loss would much rather stop their hair loss and cure their baldness. Here we talk about stem cell therapy for hair loss.
Unfortunately, there are few effective treatments for androgenic alopecia. Patients may choose to use topical medication, minoxidil. Men can use the drug finasteride. Neither of these agents is very effective for many people who try them. Some patients with pattern baldness opt for surgery. Surgical hair loss treatment can be helpful for men who have receding hairlines, but it is of little to no use in patients with diffusely thinning hair, which is most often the case in women affected by androgenic alopecia.
Scientists have turned to stem cell therapy for hair loss for a few reasons. First, the current medical and surgical treatment options are largely ineffective. Second, stem cell treatment has been shown to be safe in many scientific and clinical studies. Third and perhaps most importantly, androgenic alopecia is caused, in part, by problems with natural stem cell function. Immune cells (lymphocytes and mast cells) can be found in the area around each hair follicle, specifically in the “knot zone” which is where most hair follicle stem cells reside. These immune cells and hormonal factors likely interfere with hair follicle stem cell function—the number of hair follicle stem cells stays the same in pattern baldness, but the ability of progenitor cells to multiply is greatly reduced. Natural stem cells in people with androgenic alopecia do not produce the same levels of substances that support hair growth and renewal. In short, patients with pattern baldness may benefit from stem cell treatment.
Researchers are strenuously pursuing this line of research. One promising approach is to apply stem cells (fat and stromal vascular fraction cells) directly to the balding areas of the scalp. For example, Dr. Shin and colleagues used stem cells on 27 women with pattern baldness and showed increased hair thickness and density 12 weeks after treatment. Another approach is to use exosomes from these stem cells to treat hair loss. Exosomes are released by stem cells, contain virtually all the beneficial molecules that stem cells produce and can be applied to the scalp without surgery.
The field of stem
cell treatment for pattern hair loss is growing rapidly. As more clinical
trials are published, we move closer to a time in with stem cell and stem cell
exosome treatment for androgenic alopecia becomes a reality.

by admin | Nov 13, 2019 | Stem Cell Research, Exosomes, Mesenchymal Stem Cells
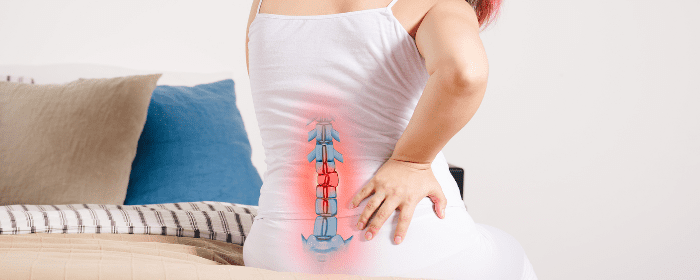
The spinal column is made up of more than a dozen vertebral bones stacked on top of each other. Since the spine is not a single bone, it is capable of pivoting and bending, which gives the torso a degree of flexibility. A key part of this structure relies on the substance between the vertebral bones called the intravertebral disc.
The intravertebral disc is made up of the annulus fibrosis (the tough outer ring) and the nucleus pulposus (the jelly-like inner core). Each intervertebral disc acts as a shock absorber between the vertebral bones. Over time and with age, however, the intervertebral disc tends to breakdown. This can cause called degenerative disc disease, which includes herniated discs (“slipped discs”), pinched nerves, neck and back pain, and nerve problems. Obviously, finding ways to reverse or prevent intravertebral discs from breaking down is of great medical and scientific interest and for the countless patients with degenerative disc disease.
As with other groups interested in regenerative medicine, researchers have turned to stem cells in an effort to regenerate tissue within the intravertebral disc. One research group reported their recent success using bone marrow-derived mesenchymal stem cells. The scientists collected exosomes—very small packets filled with highly concentrated molecules such as proteins, microRNA, transcription factors and lipids—from these stem cells. In this study, researchers also collected exosomes from nucleus pulposus cells and tested the exosomes in various ways.
The researchers found that exosomes could send out signals to bone marrow mesenchymal cells and call them to the intervertebral disc. The exosomes also prompted the stem cells to become new nucleus pulposus-like cells. Conversely, exosomes from bone marrow mesenchymal cells caused nucleus pulposus cells to grow and multiply (i.e. proliferate). Finally, exosomes helped the tissue in degenerating vertebral discs to express the same genes as healthy discs.
While these results are complex, they suggest that exosomes from bone marrow mesenchymal cells and nucleus pulposus cells work together to recruit and make more healthy cells in degenerating vertebral discs. This could have profound implications for the millions of people with degenerative disc disease. If these results are confirmed in clinical trials, it would mean that exosomes could be used to prevent or reverse degenerative disc disease. We anxiously await further work in this exciting field.
Reference: Kang L. et al. (2017). Exosomes as potential alternatives to stem cell therapy for intervertebral disc degeneration: in-vitro study on exosomes in interaction of nucleus pulposus cells and bone marrow mesenchymal stem cells. Stem Cell Research Therapy. 2017; 8: 108.

by admin | Oct 11, 2019 | Mesenchymal Stem Cells, Exosomes, Osteoarthritis
The field of Regenerative Medicine has shown great promise for helping those with a variety of chronic diseases, including arthritis. Indeed, data on the potential value of using stem cells to address issues relating to arthritis have been growing. While specific stem cells like mesenchymal stem cells have demonstrated therapeutic effects in models of arthritis and other inflammatory diseases, the specific ways in which these cells confer their benefits are not yet well understood. Given that these stem cells contain different types of elements, it is important that research establishes which of these elements is critical to the therapeutic properties of stem cells.
A recent study, published in Theranostics, looked specifically at the different effects that small exosomes and larger microparticles from within mesenchymal stem cells have on the inflammatory processes that occur in arthritis. To conduct their experiment, scientists isolated the exosomes and microparticles from mesenchymal stem cells using an ultracentrifugation technique and then exposed the exosomes and the microparticles to cells of the immune system – specifically, T and B lymphocytes, which are implicated in arthritis.
What the researchers found was that, in their models of arthritis, both the exosomes and the microparticles suppressed the T lymphocyte proliferation that is indicative of inflammation. However, unlike microparticles and even parental mesenchymal stem cells, the exosomes were also able to induce other anti-inflammatory effects. The result of exosome activity was, therefore, more efficient blunting of inflammation.
These results point to the potential of not just stem cells, but specifically the exosomes of these cells, in therapeutically addressing inflammatory arthritis. While more research is needed to understand how these exosomes could actually impact arthritis patients, these data provide hope that stem cells and even just elements of stem cells will help these patients by improving their ability to combat problematic inflammation.
Reference: Cosenza, S. et al. (2018). Mesenchymal stem cells-derived exosomes are more immunosuppressive than microparticles in inflammatory arthritis. Theranostics, 8(5), 1399-1410.

by admin | Oct 3, 2019 | Exosomes, Stem Cell Therapy
Much of the medical research and clinical applications of stem cell therapy have thus far focused on stem cells and their potential to repair damaged or diseased tissue that has not responded to conventional therapies. Though there has been a lot of evidence to suggest that the use of certain types of stem cells can be safe, experts have suggested that strategies for therapy using exosomes that can avoid the use of living stem cells may provide an even better opportunity to slow the progression of various diseases.
Paracrine secretions have been shown to play a significant role in the ability of stem cells to improve disease conditions, and exosomes are a key element of these secretions. From a functional standpoint, exosomes enable stem cells to transfer their genetic information to other cells residing in the damaged tissue.
Because these are responsible for some of the critical benefits of stem cells, researchers have speculated that the use of exosomes rather than stem cells may provide specific advantages in some therapeutic contexts. A review in Stem Cells International has provided a comprehensive overview of what is known so far about the potential role of exosomes in stem cell therapy.
Exosomes are released from a wide variety of stem cell types and influence the functioning of nearby cells and tissues. Their use alone may offer better therapeutic results. Indeed, they have shown particular promise in addressing symptoms of many conditions.
Researchers are hopeful that exosomes will be able to help patients in new and innovative ways, more research is needed to determine the best way to apply them in stem cell therapy.
Reference: Han, C. et al. (2016). Exosomes and their therapeutic potentials of stem cells. Stem Cells International, 1-11.

by admin | Aug 19, 2019 | Exosomes, Stem Cell Research, Stem Cell Therapy
Given the limitations of several conventional methods to treat a wide variety of diseases and injuries, stem cell therapy has begun to gain in popularity. The evidence supporting the field of Regenerative Medicine, which involves using stem cells to regenerate healthy, functional tissue, has indeed been accumulating in recent years.
There are a number of different types of stem cells that have been explored for their therapeutic potential. Mesenchymal stem cells have become a preferred option for therapy because of their ability to differentiate into several different types of adult tissue and to be transplanted safely and effectively into patients.
One-way mesenchymal stem cells confer their therapeutic benefits is through paracrine effects that are achieved by the secretion of extracellular vesicles, some of which are exosomes. Exosomes are between 30 and 100 nanometers (nms) in diameter and exist in blood, cerebrospinal fluid, and other bodily fluids.
A recent review, published in Cell Transplantation, covered research showing that mesenchymal stem cell exosomes are therapeutically advantageous for the management of several conditions, including Parkinson’s disease, osteoarthritis, and stroke.
The review discusses, for instance how in models of Parkinson’s disease, exosomes have been shown to provide neuroprotection. MSC-derived exosomes also appear to inhibit inflammation in the context of osteoarthritis and also to stimulate repair in damaged tissue. Further, specific exosome biomarkers, miR-9 and miR-124, have proven to be promising in diagnosing the severity of stroke.
Based on recent research covered in this review, stem cell-derived exosomes have significant therapeutic potential. Though this review focuses specifically on the relevance of exosomes in Parkinson’s disease, osteoarthritis, and stroke, exosomes will likely provide benefits for patients in a variety of contexts and will prove to be an important part of Regenerative Medicine.
Reference
Chang, Y-H, et al. (2018). Exosomes and stem cells in degenerative disease diagnosis and therapy. Cell Transplantation, 27(3), 349-363.




 St. Petersburg, Florida
St. Petersburg, Florida
