
by admin | Apr 19, 2019 | ALS, Mesenchymal Stem Cells, Stem Cell Research
Amyotrophic lateral sclerosis (ALS) is an incurable neurologic disorder that causes muscle weakness, and disability. In ALS, nerve cells degenerate causing muscle weakness and atrophy. ALS affects the nerve cells that connect the brain to the spinal cord (upper motor neurons), and nerve cells that connect the spinal cord to muscles (lower motor neurons). While some patients with ALS will experience paresthesias (numbness and tingling), most nerves that detect sensations remain intact until the very latest stages of the disease. Over time, people with ALS may experience cognitive problems such as mild dementia, though most stay mentally sharp. Patients with ALS may also experience Parkinson’s-like symptoms, such as tremor and slowness of movement (bradykinesia). When the nerves that control swallowing or breathing become dysfunctional, ALS can become life-threatening or lethal. Damage to these nerves and muscles could lead to aspiration pneumonia, and respiratory failure, respectively.
ALS is also known as Lou Gehrig’s disease because the famed New York Yankee publicly struggled with ALS. Perhaps people alive today are more familiar with another patient who suffered from ALS, the Nobel laureate physicist, Stephen Hawking. Dr. Hawking was well known for being confined to a wheelchair and almost completely paralyzed, requiring a specialized computer interface to communicate.
There is no specific treatment for ALS. Therapy is aimed at controlling the symptoms of the disease. For example, patients may have a breathing tube placed in their neck (tracheostomy) and be connected to a ventilator to help support breathing. Likewise, a feeding tube in the stomach can help patients receive hydration and nutrition if they cannot safely swallow food because of neck muscle weakness. Physical therapists help patients maximize the strength and function. Certain medicines can be used to help treat muscle spasms, sleep problems, pain, and depression.
Since there is no cure for ALS, and really no specific treatment for the condition, there is considerable interest in discovering effective treatments. One of the most promising potential therapies is to use stem cells to treat ALS. Since ALS is caused by the destruction and loss of motor neurons, a reasonable treatment approach is to use stem cells that can become motor neurons and promote motor neuron growth and development.
Recently, researchers conducted two clinical trials to evaluate the safety and feasibility of using bone marrow-derived mesenchymal stromal cells to treat patients with ALS. In one clinical trial, the researchers infused stem cells intravenously, while in the other they infused the stem cells into the cerebrospinal fluid around the spine (intrathecally). Patients in both trials were followed for up to 12 months after the infusion to see if the stem cells caused side effects. During the follow-up period, there were no reports of adverse events related to the treatment. Given the success of these trials, this work clears the way for future clinical trials to study the efficacy of stem cells for treating amyotrophic lateral sclerosis.
Reference: Nabavi et al. (2019). Safety, Feasibility of Intravenous and Intrathecal Injection of Autologous Bone Marrow-Derived Mesenchymal Stromal Cells in Patients with Amyotrophic Lateral Sclerosis: An Open-Label Phase I Clinical Trial. Cell Journal. 2019 Jan;20(4):592-598.

by admin | Oct 24, 2018 | Health Awareness, ALS, Multiple Sclerosis
Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease) and multiple sclerosis (MS) are similar in that they are both neurodegenerative disorders which impact the brain and central nervous system. Neither condition has a known cure, and both affect the muscles and nerves. Yet, the conditions have distinct difference between MS and ALS, particularly in terms of their symptoms. Here, we explore the ways in which these conditions are similar and then examine their distinctive qualities.
Similarities
Muscle Weakness: Weakness in the muscles of the arms and legs are common in both ALS and MS, as are difficulty walking and involuntary muscle spasms.
Speech Challenges: Slurred speech, while less common in MS, can be experienced by patients with both conditions. In ALS, this symptom worsens progressively, but it can be intermittent in people with MS.
Swallowing Problems: Dysphagia, or difficulty swallowing, is a symptom shared by both conditions. However, while it becomes progressively worse in patients with ALS, individuals with MS experience it to a lesser degree and intermittently.
Breathing Issues: ALS is characterized by the breaking down of the nerve cells in the brain and spinal cord, which control the muscles in your body. Thus, as muscles begin to atrophy, breathing complications become more pronounced. In people with MS, lung function is lower than normal, but shortness of breath is typically only noticed upon exertion, if at all.
Differences
Both ALS and MS scar the covering of the nerve fibers, but this happens differently in each condition. In MS, the myelin sheaths, coverings which protect the body’s nerve cells, are compromised. This impedes the brain’s ability to send signals to other parts of the body, which affects both voluntary and involuntary muscle movement. The symptoms of ALS, on the other hand, all involve nerves that control voluntary muscle movement.
The early stages of ALS vs MS Symptoms bear similarities to one another, like fatigue, trouble walking, muscle stiffness, and twitching are common in both. Yet, physicians are able to distinguish among the two fairly quickly, due to the following distinct symptoms.
Vision Impairment: While ALS sufferers may notice challenges with voluntary muscle movement, they often do not lose the ability to see. For MS patients, however, the optic nerve can become swollen, resulting in vision problems. In fact, up to 80% of all MS patients experience vision-related symptoms.
Bladder/Bowel Issues: Issues with involuntary muscles can present bladder challenges, including incontinence, in at least 80% of people with MS. Diarrhea is also common for MS sufferers. People with ALS may not experience either condition, but constipation is common in both illnesses.
Tingling/Pain: A select population of ALS patients experience tingling, but it is often temporary. For people with MS, however, sensory symptoms are common and pronounced. Numbness, tingling, and pain are reported by MS patients.
While the symptoms described above are commonly associated with ALS, MS, or both, having one or more of these symptoms does not mean a patient is afflicted with either condition. With that being said, it is always a good idea to have a physician weigh in on any new or unfamiliar symptoms to receive an accurate diagnosis and treatment plan.

by admin | Aug 28, 2018 | Stem Cell Research, Stem Cell Therapy
The evidence for the promise of mesenchymal stem cells in regenerative medicine has been growing for several years. With new sources regularly emerging, stem cells can come from a large variety of sources. Postnatal mesenchymal stem cells appear to have the most promise in regeneration. A new review has addressed how mesenchymal stem cells can be used with innovative scaffolding engineering approaches to improve techniques in regenerative medicine.
Mesenchymal stem cells are, on their own, good candidates for regeneration because of a number of characteristic features. For instance, they can differentiate into many different types of cells. Osteoblasts and chondroblasts are two cell types that mesenchymal stem cells differentiate into and that can be supported in bone regeneration by 3D-printed biomaterials like scaffolds.
Mesenchymal stem cells also can have beneficial impacts on the immune system. Unlike with other stem cell types, the severe immune reactions that may occur with the transplantation of foreign materials into the body can often be avoided with the use of mesenchymal stem cells, making them a safe option in regenerative medicine.
The current review addresses the ways in which bone regeneration can be optimized through the use of mesenchymal stem cells and scaffold engineering and how new concepts in bioengineering may be able to improve regenerative medicine in combination with mesenchymal stem cell approaches. Future research will need to focus on how we can customize regenerative approaches using what we know about mesenchymal stem cells and the most cutting-edge innovations in bioengineering.

by admin | May 7, 2018 | ALS, Stem Cell Research
Stem cells are being increasingly used to create therapies to address diseases across a number of organs. Neurodegenerative disease is one category for which there has been an abundance of research into the potential of stem cells to slow symptom progression or reverse symptoms altogether. For some neurodegenerative diseases, such as Parkinson’s disease, the approach for using stem cells is to create a therapy that enables the cells that are lost through the disease to be replaced by new cells. It is the hope of scientists and clinicians that this type cell replacement therapy will halt aspects of the disease that result from cell loss.
Recently, scientists published experimental results in PLoS One that demonstrate the potential of another type of stem cell approach. More specifically, these researchers showed that in the case of amyotrophic lateral sclerosis (ALS), using stem cells to help create a protective environment for existing cells may have a positive impact on disease progression. The specific type of stem cells used in this experiment was the mesenchymal stem cell.
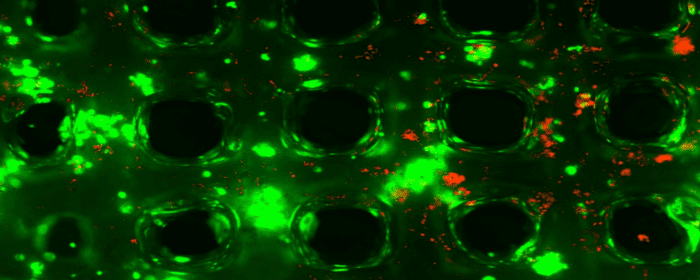
While cell replacement therapies often employ mesenchymal stem cells because of their ability to differentiate into many different cell types, the researchers in this study used them because of their promise for enhancing the health of a cell environment. Indeed, these cells are known to have immunomodulatory properties and to fight inflammation.
The researchers specifically looked at how mesenchymal stem cells could affect motor neurons and glia because these are the cell types that are implicated in ALS. What they found was that these stem cells were able to reduce apoptosis, a process whereby cells self-destruct as a result of cues in the environment that alert the cells to unhealthy conditions. Critically, the extent to which this type of cell destruction was minimized depended on the amount of mesenchymal stem cell that was present. In other words, with more stem cells came more protection.
Another important observation was that mesenchymal stem cells were associated with the expression of important growth factors that are known to support healthy environments and to reduce markers of inflammation, which tend to be associated with unhealthy environments.
Together, these results suggest that ALS could potentially be addressed with stem cells without the development of aggressive cell replacement therapies. Instead, stem cells could be used to create protective environments for neurons that are normally affected by the disease.

by admin | Jan 11, 2018 | ALS, Stem Cell Research
Amyotrophic lateral sclerosis, known as ALS, is only partially understood, and there is no effective prevention or treatment of the disease. Those who are diagnosed with ALS, therefore, have few options for slowing its progression. The disease attacks cells of the nervous system called motor neurons. Thus, while one option for approaching ALS is to prevent the attack of motor neurons, another approach is to find a way to protect those cells of the nervous system.
Small proteins called neurotrophic factors have previously been shown to help motor neurons grow and survive longer. However, when scientists have tried to apply these neurotrophic factors in ALS patients, they have not made a difference in disease progression. Because stem cells offer a way to replace damaged cells, they are studied as potential candidates for therapeutic interventions in neurodegenerative diseases, such as ALS.
In this study, scientists combined stem cells and neurotrophic factors by inducing mesenchymal stem cells to secrete neurotrophic factors. Their main objective was to determine if injecting this type of stem cell into ALS patients is safe. They also aimed to determine if such cells may be clinically helpful for this group of patients.
The scientists gave 6 patients each the stem cells through two different types of injections. They then gave 14 patients a combination of the two types of injections. All patients were between the ages of 20 and 75 and were in the early stages of ALS. The patients were observed for 6 months following their injections. Any side effects that occurred as a result of the stem cell injections were mild or transient, so each of the techniques for administering the stem cells to ALS patients was deemed safe.
The researchers also used a test called the ALS-Functional Rating Scale-Revised to evaluate the clinical impact of the stem cell treatment on ALS patients. They found that 13 of the patients (or 87%) improved in their performance on the test, suggesting that the stem cells may have improved ALS symptoms. Further research will need to be conducted to determine if these mesenchymal stem cells that secrete neurotrophic factors can indeed help ALS patients – and if so, how they can best be used to combat the disease.



 St. Petersburg, Florida
St. Petersburg, Florida
