
by admin | Oct 8, 2018 | Health Awareness
Neurological disorders affect the central nervous system, including the brain, spinal cord, and/or peripheral nerves. These conditions can impede speech, movement, learning, and even vital functions such as breathing and swallowing. They may also impact a person’s mood, senses, and memory. For individuals with these types of conditions, physical therapy (PT) can be a powerful component in a robust and individualized treatment plan.
While there is no cure for conditions like multiple sclerosis, Alzheimer’s disease, and Parkinson’s disease, treating the symptoms associated with these conditions can aid promote functionality, pain management, and overall quality of life. Here, we take a closer look at the role of physical therapy (PT) plays in the managing neurological disorders.
Minimize Symptoms
PT can be used to proactively minimize symptoms and slow their progression. Neurological physical therapy can reduce motor defects that impair nerve cell functionality through specific exercises. Before a patient experiences motor loss, physical therapy may help an individual stay fit and mobile.
Regain Functionality
Once symptoms do occur, the focus of PT shifts to helping a person relearn motor skills. Advanced neurological therapy may include balance and exercise activities, compensatory strategies to perform daily tasks, use of therapy equipment such as splints or braces, and gait training with the use of assistive devices. Therapy for speech, language and swallowing can also be provided as needed.
Preserve Skills & Abilities
After individuals with neurological conditions have regained skills or developed adaptive means, they can attend PT on an ongoing basis to preserve their abilities. PT programs can assist neuroadaptive and neuroprotective processes to support independence and social participation for patients even after symptoms have begun to impact their lives. In combination with other treatments such as medications and alternate forms of therapy, PT support an optimal quality of life for people with neurological disorders.

by admin | Oct 4, 2018 | Stem Cell Therapy, Lupus, Wharton's Jelly
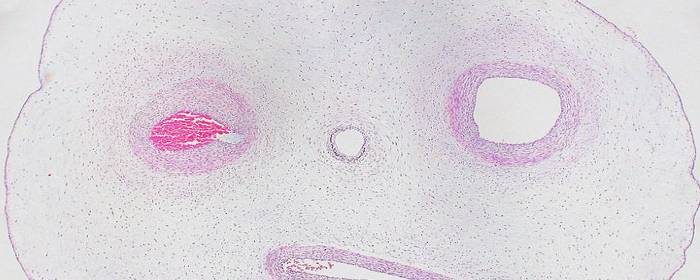
Wharton’s jelly is a rather unique body fluid. It is the connective tissue found within the umbilical cord. While Wharton’s jelly is connective tissue, it more closely resembles gelatin. Historically this material was discarded as medical waste; however, Wharton’s jelly has been shown to contain a number of therapeutic substances. Among these healing substances found within Wharton’s jelly is an abundant supply of mesenchymal stem cells.
One of the most intriguing features of Wharton’s jelly is that it contains a virtually limitless supply of mesenchymal stem cells. There are about 4 million new births in the United States each year, 5 million in the European Union, and over 100 million worldwide. The potential pool of cells is staggering when you consider only a small amount of Wharton’s jelly can contain millions of stem cells. Notably, Wharton’s jelly is usually discarded after the delivery of a healthy baby. If this material could be donated instead of discarded, researchers believe they have found an abundant, renewable resource from which to draw mesenchymal stem cells.
However, the abundance of Wharton’s jelly is not the most impressive feature of the substance. The stem cells found in Wharton’s jelly are rather unique. Perhaps most importantly, the cells are immuno-privileged. This means they are not readily recognized by the immune system. Consequently, the stem cells can be taken from the umbilical cord, purified, and then injected into a patient with little risk of the patient having an immune reaction to the cells. These particular mesenchymal stem cells are also interesting because they are relatively “primitive,” which means they have some of the same properties of embryonic stem cells. However, Wharton’s jelly can be obtained without controversy, while harvesting embryonic stem cells from aborted tissue remain highly controversial.
Stem cells taken from Wharton’s jelly are already being used in some clinical studies. For example, researchers in one clinical study injected type 2 diabetes patients with Wharton’s jelly-derived mesenchymal stem cells. Within six months of treatment, 7 of 22 patients became insulin-free and 5 were able to reduce the amount of insulin they needed by more than 50%. Only one patient out of the 22 did not respond to the stem cells at all. The cells have also been tested in systemic lupus erythematosus, better known as simply lupus. Forty patients received Wharton’s jelly mesenchymal stem cells intravenously. Thirteen patients enjoyed a major clinical response while 11 enjoyed a partial clinical response of their lupus symptoms.
As more clinical studies are done on Wharton’s jelly-derived mesenchymal stem cells, we will learn what other diseases can be treated with this once-discarded substance. Early indications show a very promising future.

by admin | Oct 3, 2018 | Health Awareness, Stroke
Stroke is a serious, life-threatening condition in which the blood supply to the brain is interrupted or diminished, often resulting in permanent brain damage and disability. While nearly 800,000 people experience a new or recurrent stroke each year, these conditions are largely preventable. In fact, up to 80% of all strokes can be prevented.
Part of prevention comes from knowing to understand your risk factors. There are many factors contributing to the condition, including lifestyle, medical, and genetic factors, which are explored below.
Lifestyle Risk Factors
Smoking: Smoking can damage the blood vessels in many ways, causing thickening and narrowing and increasing the buildup of fat. This makes it more difficult for blood to get through, which can eventually lead to conditions like stroke and heart disease.
Being Overweight: Excess body weight produces similar effects: it can increase blood pressure and spike cholesterol levels, so exercising regularly and eating a diet consisting mostly of unprocessed foods can help to minimize your risk factors.
Heavy/Binge Drinking: A recent study linked frequent binge drinking to specific cardiovascular risk factors known to cause stroke, including high blood pressure, cholesterol, and blood sugar, at a younger age. The Stroke Association recommends limiting alcohol consumption to two drinks per day for men and one drink per day for women.
Medical Risk Factors
High Blood Pressure: High blood pressure puts physical pressure on your blood vessels, which can cause them to narrow, rupture, leak, or experience clots. Luckily, high blood pressure can now be controlled successfully through medications and lifestyle changes.
Diabetes: Type 2 diabetes is an independent risk factor for stroke, but when coupled with being overweight and having high blood pressure (which most patients with the disease have), the correlation is even stronger. Managing diabetes is critical to reducing risks of other serious conditions, including heart disease and stroke.
Other Risk Factors
Sex: Each year, more women than men have strokes. Certain factors such as pregnancy, gestational diabetes, oral contraceptive use (especially when combined with smoking), and hormone therapy can impact risk, so be sure to discuss your women’s health history with your physician.
Age: Individuals over the age of 55 are more likely to suffer a stroke than younger individuals. For this reason, minimizing risk factors wherever possible and maintaining regular preventive care appointments with physicians is essential in older adults.
Personal/Family History: If you’ve previously suffered a stroke or heart attack, or if someone in your immediate family has, you may face a higher risk of stroke. Individuals who have experienced cardiac issues should maintain the preventive care treatment plan recommended by their cardiologist.
While stroke isn’t always preventable, having even a basic understanding of these principles can help you maintain awareness and seek the right preventive care to help reduce your risk.

by admin | Oct 1, 2018 | Health Awareness
Certain types of food are commonly known to trigger inflammation in people who are sensitive to specific agents. To manage diseases such as irritable bowel syndrome, Crohn’s disease, and other chronic inflammatory disorders, many people have turned to the low-FODMAP diet.
What Does FODMAP Mean?
FODMAP is an acronym for fermentable oligo-, di-, monosaccharides and polyols. In short, they are dietary sugars found in many grains, types of produce, and dairy products. While these FODMAPs sound complex, they simply refer to characteristics in foods that are known to present digestion challenges. These agents are highly fermentable, and it is their rapid fermentation that leads to bowel issues. For instance, they create an osmotic effect, meaning they draw water through the bowel, creating increased permeability. They are also poorly absorbed within the small intestine, and the fermentation that takes place within can create gas, abdominal pain, discomfort, diarrhea, and constipation.
Which Foods are Considered High-FODMAP?
There are many foods high in FODMAPs. Foods with excess fructose, including honey, dried fruit, watermelon, pears, and apples, should be avoided on the diet. Sources of lactose, including milk, yogurt, and dairy desserts, are also high-FODMAP. Leeks, onions, barley, rye, wheat, garlic, legumes, cashews, and chickpeas are best avoided on the diet as well. This list is by no means exhaustive, however, and there are many other foods considered to be high enough in FODMAPs to cause an inflammatory response. With that said, certain food sources don’t have to be avoided entirely on the diet and limiting portion sizes may be enough to minimize inflammatory effects.
Is the Low-FODMAP Diet Right for Me?
Because many high-FODMAP foods are also rich sources of key nutrients, it is typically not recommended for anyone who doesn’t have an apparent sensitivity to FODMAPs to try the diet. Avoidance of FODMAPs could put individuals at risk of nutritional deficiencies, as it restricts many healthy foods. Thus, it should only be followed as prescribed by healthcare professionals.
In fact, this restrictive diet is only practiced for three to eight weeks at a time. It is typically followed in phases. The first phase involves strict elimination of FODMAPs, followed by a reintroduction stage during which one type of FODMAP is introduced at a time. This allows patients to gauge which group triggers the most significant inflammatory response. Then, in the final phase, the modified FODMAP diet can be followed, in which certain trigger foods can be avoided at the patient’s discretion.
While a low FODMAP diet is not intended to be a permanent solution, it can shed light on which dietary sources elicit the most challenging symptoms in disorders like IBS and Crohn’s disease. If you’re interested in exploring the eating plan to help you manage your condition, be sure to speak with your gastroenterologist to discuss your eligibility for the diet.

by admin | Sep 27, 2018 | Heart Failure, Stem Cell Therapy
People with heart failure may have trouble breathing, walking, and having a normal life. Current treatments for heart failure are aimed at making the healthy heart tissue pump harder (e.g. digoxin). On the other hand, treatments largely ignore dead heart tissue because there A myocardial infarction, better known as a heart attack, occurs when blood flow through the coronary arteries to the heart is blocked. This usually occurs when a blood clot forms in a coronary artery. Since the heart is a highly active muscle, it requires a constant supply of oxygen and nutrients to maintain its pumping function. When the heart muscle is starved of oxygen, as is the case during myocardial infarction, heart cells become dysfunctional. If blood flow through the coronary arteries (which carries oxygen to the heart) is not restored soon after a heart attack begins, those dysfunctional heart cells will die.
When heart tissue has been destroyed by a heart attack, patients are usually left with poor heart function. This can lead to congestive heart failure. One way to determine whether someone who has had a heart attack has suffered lasting heart damage is to perform an echocardiogram, or simply an “echo.” By performing an echo, doctors can estimate the heart’s ability to pump blood by measuring left ventricular function.
has been no known way to rescue it. With the discovery and use of stem cells, however, there is a chance that scientists may be able to rescue dead heart muscle and improve cardiac function.
In a study, researchers blocked the coronary arteries of experimental animals to cause myocardial infarction. Four weeks later, they injected either bone marrow-derived stem cells or adipose-tissue-derived stem cells into the heart. Impressively, blood flow significantly improved to the heart and heart function. Treated animals had substantially higher left ventricular ejection fraction, essentially reversing heart failure a full month after a heart attack. Shockingly, the researchers found that stem cells appeared to salvage dead heart tissue, meaning that the size of the damaged area was smaller after treatment.
While these incredible results will need to be replicated in humans, this research represents an exciting breakthrough in cardiology and regenerative medicine. The stem cell approach may be able to help patients who have had a heart attack, but could not get medical treatment in time to remove the clot.




 St. Petersburg, Florida
St. Petersburg, Florida
