
by Stemedix | Mar 15, 2021 | Traumatic Brain Injury, Stem Cell Therapy
Traumatic brain injuries (TBI) occur from an outside force, and are commonly caused by sports injuries and car accidents. In many cases, symptoms can improve over time with the help of therapy. In some cases, however, it’s possible for symptoms to worsen over time. Here’s a closer look at why some cases improve and others appear to decline.
Secondary Brain Injury: In certain patients, complications develop after the initial injury, such as an infection or hematoma. The injury may also cut off blood to the brain, causing brain cells to die. The effects of these secondary brain injuries may not appear right away, which is why some patients’ symptoms seem to worsen over time.
Chemical Events: A brain injury can also trigger chemical changes which lead to worsening symptoms. For instance, the patient may develop an abundance of neurotransmitters, causing brain cells to become overstimulated and eventually die off.
Failure to Receive Treatment: Lastly, if a patient fails to receive proper treatment to facilitate healing following their brain injury, their symptoms are likely to worsen.
How to Minimize the Risk of Worsening Symptoms
Experts don’t know why symptoms worsen in some TBI cases and not others, but there are still factors within your control that can promote optimal outcomes. Here are a few options to consider.
Attend Therapy
Many people recovering from TBI need a combination of physical, speech, and occupational therapy. These rehabilitative programs help you rebuild physical strength, support blood flow to the brain, sharpen your mental skills, and reestablish your daily routine. Most importantly, they keep the brain and body active and can help prevent worsening symptoms.
Keep Your Brain Stimulated
Your brain is a muscle that can benefit from regular exercise. If there’s a type of puzzle you enjoy, such as sudoku or crosswords, try doing some during your downtime. You might also consider music or art therapy to engage your brain. Stimulating your brain encourages it to produce neuropathic growth factors, which kickstart the development of brain cells. Of course, you’ll want to follow your practitioners’ recommendations and avoid overstimulation during early recovery.
Engage Your Neuroplasticity
Neuroplasticity is the mechanism the brain uses to create neural pathways which allow healthy brain tissue to take on functions the damaged portions can no longer accommodate. Repetition is one of the simplest yet most effective ways to engage neuroplasticity. Thus, if there’s a skill you want to remaster, you’ll need to practice it often. Over time, it will start to become easier.
Get Support
TBI recovery can be frustrating, especially if you’ve reached a plateau. Support groups are available to encourage you to overcome plateaus and discuss the ups and downs with first-hand knowledge. Whether you choose to join an online community or meet with a group in person, you may find that sharing your experiences in a supportive setting is a great outlet for the emotional and mental challenges that come with recovery.
Although it’s impossible to say for sure whether someone’s TBI symptoms will worsen or improve with time, the steps above won’t hurt in either case. By staying mentally and physically active and pursuing treatments such as therapy, individuals who have experienced brain injuries can support the best possible outcomes in their recovery. Patients are discovering the alternative option of stem cell therapy to help manage symptoms and assist in the healing process. In particular, stem cells can slow or halt further brain damage and promote healing by reducing inflammation and achieving a tissue-protective effect. If you would like to learn more then contact us today to speak with a care coordinator.

by Stemedix | Jan 4, 2021 | Traumatic Brain Injury
The brain controls everything we do, including our emotions, behaviors, the way we move our bodies, how we process information, and how we interact with others. As such, a traumatic brain injury can have life-altering effects, not only for the person who sustains it but also for their loved ones.
Every brain injury is different, and the precise circumstances that unfold afterward will depend on several unique factors, including the location and severity of the injury. Some impairments are primary, which means they are directly related to the injury itself and are usually physical and cognitive in nature. Others, such as emotional and behavioral changes, can be both primary and secondary impairments.
Here are a few of the changes you could expect to see in a person who has experienced a brain injury.
Physical Changes
Nearly all brain injury survivors report feeling fatigued, especially soon after the event. An injured brain has to work much harder to perform normal functions, so long stretches of sleep are common in people as they’re healing, sometimes even indefinitely.
Other physical changes could include muscle weakness, headaches, partial paralysis, persistent pain, sleep disturbances, spasticity, seizures, speech and swallowing differences, and appetite changes to name a few. Some physical changes are permanent, while others can be addressed through physical therapy, medications, and if needed, surgeries.
Cognitive Changes
The cognitive impairments a survivor sustains are often among the most disabling of all the effects. They are most intense immediately after the injury, and while they may improve significantly, it’s rare that they disappear fully. With that being said, recovery can be an effort that span’s a person’s entire life, with improvements being made all the time.
Memory impairments are particularly common in brain injuries. Both the short- and long-term memory may be affected, as well as retrograde (events before the injury) and anterograde (events after the injury). A person may also face challenges in certain areas such as learning new material and processing information, comprehending language, safety awareness, spatial orientation, judgment and decision-making, comprehension, attention, and concentration.
A person’s executive functioning, including activities surrounding planning, organizing, multi-tasking, evaluating, and problem-solving, can also be affected.
Communication Changes
The communication changes a person may experience can span far and wide. For instance, they might struggle with speech as well as the ability to understand and process words. Reading impairments, difficulty finding the right word, and a limited listening attention span may also develop.
Emotional Changes
Emotional impairments can occur from the brain injury itself, or as a result of a primary impairment. For instance, someone might experience depression as a reaction to the physical or cognitive challenges they’re facing. A few emotions people can have after a brain injury are anger, apathy, anxiety, paranoia, frustration, confusion, restlessness, post-traumatic stress, and mood swings. Oftentimes, emotional challenges can be addressed through therapy.
Behavioral Changes
Like emotional changes, behavioral differences can be directly or indirectly caused by brain injury. They can range from mildly irritating to dangerous. Some behavioral changes that could emerge are withdrawal, verbal or physical aggression, intolerance, over-or under-reactions, rebelliousness, defensiveness, and excessive crying.
Behavioral changes call for patience and understanding from an individual’s support system, but those with potentially dangerous consequences should be addressed in an inpatient environment.
Social Changes
Many people experience feelings of loneliness following a brain injury. The largest population of survivors is young men, whose friends may not understand the wide range of changes they’re experiencing. Oftentimes, survivors’ friendships, and romantic relationships suffer. Issues like behavioral and emotional changes, difficulties with conversations and understanding social cues, and fatigue, can impact social lives. Nonetheless, many survivors get tremendous support from their families and are ultimately able to enjoy loving relationships and fulfilling friendships.
Family Support
Survivors’ family members will face stress and their own range of emotions after their loved one experiences a brain injury. Everyone handles the event and recovery in their own ways, and the challenges they face will depend on a number of independent factors.
Children, in particular, should be encouraged to openly discuss their feelings. If emotions among family members seem particularly intense, counseling could help.
Parents should consider how they’ll divide time between caring for the family, the survivor, and managing other responsibilities, such as work and household management. While there will be a lot to juggle, resources are available for support, such as BrainLine.org and the Brain Injury Association of America.
If you are interested in regenerative medicine also know as stem cell therapy for brain injuries then contact a care coordinator today for a free assessment!

by Stemedix | Aug 1, 2020 | Stem Cell Therapy, Traumatic Brain Injury
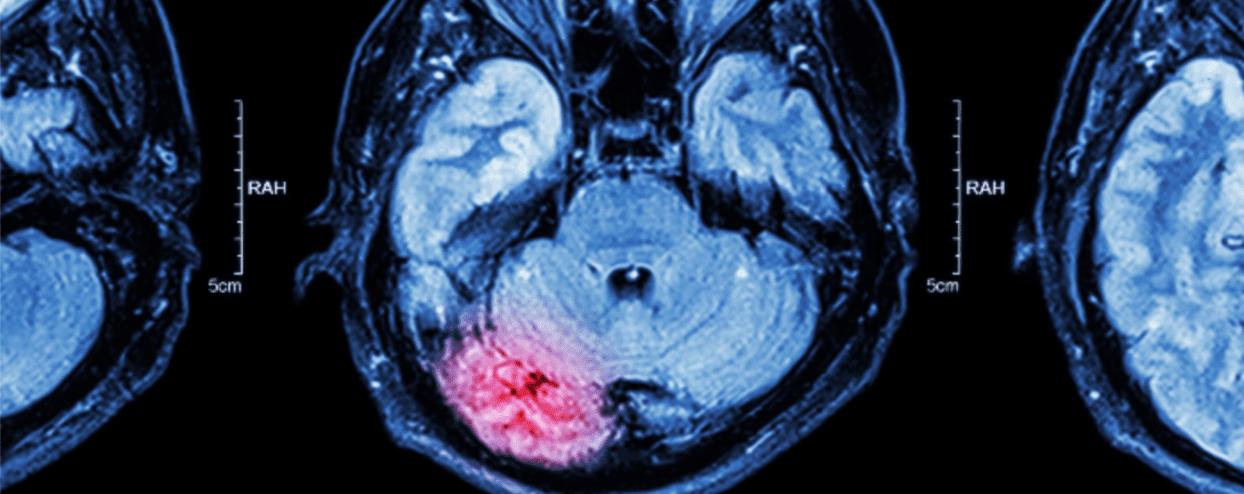
Traumatic brain injury (TBI) occurs when sudden trauma damages the brain. While mild TBI can temporarily affect brain cells, more serious injuries can lead to bleeding, torn tissue, and bruising which can cause lasting complications. Brian damage studies have shown that stem cells may be an alternative option for patients to explore.
According to research, exogenous stem cells can target damaged brain tissue. They can then partake in the repair process by differentiating into cells that replaced the damaged tissue, while simultaneously releasing anti-inflammatory properties. These effects have the ability to promote improvements in neurological function in people with TBI.
Several types of stem cells have been studied for TBI, including:
- Mesenchymal Stem Cells: Typically retrieved from adult bone marrow, mesenchymal stem cells (MSCs) aid in tissue regeneration, the inhibition of inflammation, and the recruitment of progenitor cells to replace lost cells. Other studies have shown improvement in neurological function after MSC treatment was administered.
- Neural Stem Cells: Neural stem cells (NSCs) self-renew and can differentiate into different types of cells, including neurons. According to results from animal studies, transplanted NSCs were able to mature into different brain cells and survive for at least five months. Studies have also shown that NSC injection enhances cognitive and learning abilities, as well as motor function.
- Multipotent Adult Progenitor Cells: Known for their ability to differentiate into endothelial cells, multipotent adult progenitor cells (MAPCs) have been shown to improve memory retrieval, the ability to retain information, spatial learning, and dyskinesia (impairment of voluntary movement). These cells have particularly powerful anti-inflammatory response characteristics.
- Induced Pluripotent Stem Cells: In 2007, Japanese scientists reprogramed somatic cells into a new class that resembled embryonic stem cells, known as induced pluripotent stem cells (iPSCs). Using the TBI model, researchers have determined that iPSCs could improve neurological function after transplanted into the injured area and specifically enhance motor function.
- Endothelial Progenitor Cells: Endothelial progenitor cells (EPCs) are the precursors of vascular endothelial cells found in the bone marrow. They are recruited to the site of injury, especially after brain injury. In a brain injury model, endothelial colony-forming cells (ECFCs) showed an ability to home in on the injured area and repair the blood-brain barrier. They can enhance capillary formation and reduce inflammation.
While further research is needed on these methods of stem cell therapy, early results do show promise in their benefits for those exploring regenerative medicine options for Traumatic Brain Injury. Contact a Care Coordinator today for a free assessment!

by admin | Jun 26, 2020 | Traumatic Brain Injury, Exosomes, Stem Cell Therapy
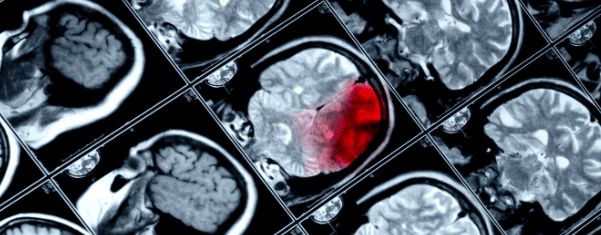
Traumatic brain injury is a single name given to a broad variety of conditions. In every instance of traumatic brain injury, some external force causes damage to the brain. This may be mild and short-lived, such as a concussion, or severe and permanent, such as severe head trauma. The initial trauma or injury can cause a number of injuries to the skull and brain such as skull fracture, cerebral contusion (“brain bruise”), cerebral edema (“brain swelling”), or hemorrhage (“brain bleed”).
Traumatic brain injury can also cause several secondary injuries that may continue for hours or days. The secondary effects of traumatic brain injury include:
- Electrolyte imbalances
- Mitochondrial dysfunction
- Inflammation
- Ischemia (lack of blood flow to parts of the brain)
- Brain cell destruction
These secondary traumatic brain injuries can cause long-term and even permanent neurological dysfunction.
Unfortunately, there are very few treatments for traumatic brain injury. Neurosurgeons can sometimes stop brain bleeding, stabilize skull fractures, and reduce brain swelling; however, there is little that can be done to stop the secondary effects of traumatic brain injury. Doctors have tried using steroids or hypothermia (cooling the patient) to decrease inflammation and stop further injury, but these interventions are not highly effective.
Ideally, one would give a treatment soon after a person has had a traumatic brain injury. This treatment would reduce or block the secondary effects of traumatic brain injury. Scientists are studying whether stem cell treatment can do that very thing.
Researchers recently showed that exosomes from bone marrow mesenchymal stem cells were able to reduce the secondary effects of traumatic brain injury. They humanely caused a traumatic brain injury in a group of mice. Fifteen minutes after the TBI, half the mice were given an injection of stem cells and the other half received a placebo (i.e. saltwater).
The mice that received the stem cell exosome treatment did substantially better than the mice who received a placebo. Stem cell exosome treatment substantially reduced the size of the damage to the brain compared to control. Moreover, mice that received stem cell exosome treatment did better on sensory, motor, reflex, and balance tests. In other words, stem cell exosome treatment helped mice with traumatic brain injury move better than those that did not receive stem cell exosome treatment.
The scientists went on to show that exosome treatment helped block the secondary effects of traumatic brain injury on the cellular and molecular level. In short, stem cell exosome treatment reduced inflammation in the brain from TBI.
Taken together, these results strongly suggest that treatment with exosomes from bone marrow mesenchymal stem cells soon after traumatic brain injury has the ability to protect the brain from damage. Of course, this treatment will need to be tested in humans who have had incidental TBI. Nevertheless, the basic science results are quite exciting since few neuroprotective agents, if any, can block the secondary effects of traumatic brain injury the way exosomes did in this scientific report.
Reference: Haoqi, N., et al. (2019). Exosomes Derived From Bone Mesenchymal Stem Cells Ameliorate Early Inflammatory Responses Following Traumatic Brain Injury. Frontiers in Neuroscience. 2019 Jan 24; 13:14.

by Stemedix | May 25, 2020 | Stem Cell Therapy, Traumatic Brain Injury
Traumatic brain injury (TBI), also known as concussion, is a common condition that affects thousands of people every year in the United States alone. The most challenging aspect of TBI is its vague clinical presentation, which makes it difficult for physicians to promptly diagnose and treat this condition without a proper history of trauma.
According to the Centers for Disease Control and Prevention (CDC), the number of TBI-related hospital visits and deaths increased by 53% between 2006 and 2014. Unfortunately, patients who survive after a concussion often deal with neurological sequela for the rest of their lives. This article will explore the basic concepts of TBI as well as the role of stem cell therapy in restoring normal neurological function after irreversible damage.
How Do Concussions Happen?
The brain is a fragile organ that’s protected by a boney structure known as the skull. Unfortunately, this protection can be a double-edged sword. To prevent contact between the brain and the skull, a liquid called cerebrospinal fluid (CSF) acts as a shock absorber to avoid any trauma to the brain when the skull is abruptly moved. In other words, the brain is floating in the CSF to be able to easily move around when you change positions.
A concussion occurs when the brain collides with the skull at an intensity that surpasses the CSF-cushioning ability. Consequently, the brain will shrink on itself, sending shock waves through the entire tissue, which tear the neurons. This phenomenon is referred to as diffuse axonal injury. As a result, the interneural network responsible for every task that the brain completes is compromised and may lead to irreversible loss of function.
Stem Cell Therapy and Traumatic Brain Injury
Stem cells have the ability to differentiate into several body tissues, which makes them a candidate to treat and repair damage for a myriad of medical conditions, including traumatic brain injuries.
In a clinical trial, researchers used bone marrow-derived stem cells as repair agents to restore the function of damaged brain tissue after enduring TBI. Stem cells were introduced to patients using minimally-invasive procedures with highly-sensitive imaging guidance to deliver the cells at the exact site of tissue damage.
Researchers stated that “These stem cells secrete growth factors that have shown preclinical benefit and also recruit the patient’s own stem cells through various homing signals. Recent successes with similar stem cell therapy trials in other diseases, such as for heart attack recovery, have generated increased interest in now using these approaches to treat brain injury.”
Moreover, a 2018 study published by nature, scientists aimed to find out if certain types of cell therapy, such as umbilical cord stem cells and bone marrow-derived stem cells benefit patients with traumatic brain injuries. The researchers found that these cells can regenerate neurons and repair damage, which may revolutionize the field of traumatology since patients may restore certain neurological functions even after irreversible damage.
Note that the idea of using stem cell therapy to treat concussions is not new, as a 2002 experimental study on rats concluded that “We show for the first time that the IV administration of human umbilical cord blood cells reduces functional deficits after severe traumatic brain injury in the rat. The injected cells enter the brain, migrate into the injured area, and a few express the neuronal and astrocytic phenotypes and integrate into the vascular structures. Cord blood administration may be a useful treatment for traumatic brain injury.”
The use of stem cell therapy to manage symptoms of TBI are still in the experimental phases; however studies have shown its potential to restore lost functions with minimally-invasive procedures that carry an extremely safe side effect profile.
Contact us today!

by admin | Apr 30, 2019 | Hyperbaric Oxygen Therapy, Stem Cell Research, Stem Cell Therapy, Traumatic Brain Injury
Traumatic brain injury (TBI) encompasses a wide range of injuries, neurological problems, and outcomes. On one end of the spectrum is a concussion, which can be mild and short lasting. At the other end of the spectrum, traumatic brain injury can be lethal or leave patients with chronic mental and physical problems. Despite this range of severities, traumatic brain injury is one of the leading causes of disability in the United States, affecting over 13 million people. People who suffer from chronic symptoms related to traumatic brain injury may struggle with chronic seizures, memory problems, concentration problems, agitation, among others. TBI can have profoundly worsened a person’s quality of life and overall well-being.
Unfortunately, little can be done to treat traumatic brain injury directly. Aside from treating symptoms, the main treatment for TBI is to have the patient to rest and avoid stimulation in an effort to give the brain time to heal. Patients can regain some function through intensive work with physical, occupational, speech, and recreational therapist. However, the brain’s ability to heal itself is limited compared to other tissues of the body. In short, the brain has very little capacity to make new brain cells after we are born. So once TBI has occurred, patients either need to depend on other healthy areas of the brain or simply adapt to their circumstances.
Fortunately, researchers are finding ways to improve on nature through hyperbaric oxygen therapy. Drs. Shandley, Wolf and other hyperbaric medicine researchers recruited a group of 28 military veterans who sustained a traumatic brain injury in Iraq or Afghanistan. These individuals had ongoing cognitive problems as a result of their brain injuries. Researchers placed some study participants in 2.4 atm avoid hundred percent oxygen, while the others simply underwent a placebo experience at basically normal pressure and oxygen levels. The two groups underwent 30 exposures each and took a cognitive test before and after these treatments.
Hyperbaric oxygen therapy increased the number of stem cells in the blood of patients with TBI. In other words, hyperbaric oxygen treatment was able to move stem cells from the bone marrow and perhaps other tissues into the bloodstream. At the same time, those treated with hyperbaric oxygen performed better on tests of cognition including ImPACT, BrainCheckers, and PCL-M test. Moreover, no adverse effects of treatment were observed. Taken together, these results suggest 30 sessions of hyperbaric oxygen treatment at 2.4 atm was able to increase stem cells in the blood and improve cognition in US warfighters who suffered traumatic brain injury during combat. These results are encouraging news for the millions of veterans and nonveterans who sustained a traumatic brain injury every year.
Reference: Shandley, S. et al. (2017). Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy. Undersea & Hyperbaric Medical Society. 2017 May-Jun;44(3):257-269.



 St. Petersburg, Florida
St. Petersburg, Florida
