
by admin | Nov 21, 2019 | Chronic Pain, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy
A review in the Journal of Stem Cell Research & Therapy has summarized an array of studies that demonstrate that a specific type of stem cell – the mesenchymal stem cell – may be beneficial as a therapeutic approach to chronic pain. The authors point to the huge burden of chronic pain. It is estimated that more than 115 people suffer from the condition, which is more than those who suffer from diabetes, stroke, cancer, and coronary heart disease combined. Many medical professionals are pondering the question of how stem cells may help those with chronic pain.
Chronic pain is also associated with significant losses in productivity. Given how extreme the burden of chronic pain has become, the National Institute of Medicine has suggested that finding effective ways to alleviate chronic pain should become a priority for the nation.
Regenerative medicine has offered an effective way to treat a variety of injuries and diseases, including some that are related to chronic pain. As the term “regenerative medicine” implies, much of the research into the clinical effects of stem cells have shown that they lead to beneficial outcomes by regenerating damaged tissue by replacing that tissue with new cells.
This new review looks at the potential of mesenchymal stem cells to specifically improve chronic pain through the ability of the cells to suppress inflammation. Given that inflammation is a common characteristic of conditions associated with chronic pain, a strategy that addresses this phenomenon could represent an effective way to help those with chronic pain that comes from things like degenerative disc disease and osteoarthritis.
The current approaches to chronic pain are limited in their ability to reduce or control pain, so there is a great need to develop more effective therapies. Research thus far into the potential impact of mesenchymal stem cells on chronic pain has provided promising results regarding effectiveness and safety. Specifically, these stem cells have not been associated with adverse side effects, they lead to the development and growth of healthy tissue, and they appear to provide pain relief. Future research will help to clarify the mechanisms by which mesenchymal stem cells may confer their benefits to those with chronic pain and provide new insights into how can best use these cells to help chronic pain sufferers.
Reference: Waterman, R.S. & Betancourt, A.M. (2011). Treating chronic pain with mesenchymal stem cells: A therapeutic approach worthy of continued investigation. Journal of Stem Cell Research & Therapy, S2, 1-5.

by admin | Nov 15, 2019 | Adipose, Heart Failure, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy
A myocardial infarction, commonly known as a heart attack, occurs when blood flow through the coronary arteries is blocked. A heart attack usually happens to people with atherosclerotic coronary heart disease, which narrows one or more of the coronary arteries. A blood clot becomes lodged in the narrowed artery, preventing blood from reaching the heart muscle. Because the heart needs a virtually constant supply of oxygen-rich blood to survive, an interruption in blood flow to the heart can quickly cause muscle cells to die. There has been much talk in the medical community of using stem cells to rebuild the heart after a heart attack.
Dead heart muscle cells cannot help the heart pump blood. Thus, people who suffer a heart attack are often left with “weak” hearts. Instead of strongly squeezing blood out of the heart to the rest of the body, a larger portion of the blood remains in the heart (i.e. reduced ejection fraction). People who have had a heart attack that reduces ejection fraction commonly develop a condition known as congestive heart failure.
People with congestive heart failure often have difficult lives. Congestive heart failure patients periodically experience exacerbations that require hospitalization. They are put on restrictive diets; their salt and fluid intakes are limited. They must also take several different medications to help the heart pump blood through the arteries to the body and keep fluid levels in the body low. These medications do not heal or replace dead heart muscle cells. Instead, they make the remaining cells work harder (or decrease resistance in the arteries, or help the body eliminate fluid through urination).
What is needed is a way to regenerate dead heart muscle cells. Fortunately, several research groups are working on ways to use stem cells to regenerate heart muscle cells so that heart attack patients can regain heart muscle function.
There have been at least 11 clinical trials studying the effects of stem cells on patients with myocardial infarction. The trials show that stem cell infusion into the vein, the coronary artery, or the heart muscle itself is safe and well-tolerated by patients. Notably among the studies, patients with acute myocardial infarction who received allogeneic human mesenchymal cells intravenously had a better ejection fraction, better heart structure, and better lung function after six months than those who received a placebo. In the APOLLO trial, patients with acute myocardial infarction who received adipose-derived mesenchymal cells had half the dead heart muscle cells than those who received a placebo (i.e. lesion volume was 50% lower in treated patients).
Phase III clinical trials are considered definitive (pivotal) evidence of benefit. In phase III C-CURE trial, patients with heart failure due to coronary artery disease received autologous mesenchymal cells (i.e. their own cells, specially prepared). Treated patients enjoyed significantly increased ejection fraction (heart-pumping ability) and better functional capacity and quality of life. Other Phase II clinical trials (ADVANCE, CONCERT-CHF, TRIDENT, POSEIDON-DCM) are ongoing.
These results are welcome news for patients who suffer—or will one day suffer—from a heart attack, an event that happens in 735,000 Americans every year.
Reference: Golpanian, S. et al. (2016). Rebuilding the Damaged Heart: Mesenchymal Stem Cells, Cell-Based Therapy, and Engineered Heart Tissue. Physiological Reviews. 2016 Jul; 96(3): 1127–1168

by admin | Nov 7, 2019 | Stem Cell Research, Adipose, Stem Cell Therapy
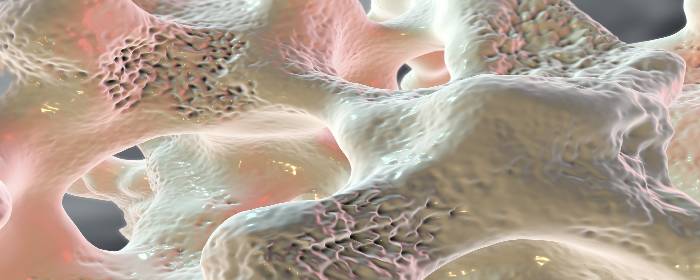
Osteoporosis is a disease in which bones become weak, brittle, and are prone to fracture. While osteoporosis is commonly considered a disease of low bone density, it is more complex and extensive than that. New bone is constantly formed and destroyed (resorbed) throughout life. In osteoporosis, however, the rate at which it is resorbed accelerates, while the rate at which it is formed slows down. In other words, bone is being destroyed faster than it can be formed. This process changes the size and shape of bones and alters its microarchitecture (i.e. the structure of bone on a microscopic level).
Without screening, most people will not know that they have osteoporosis until they have a bone fracture. Bones simply get weaker until some minor trauma causes one or more bones to break. Fortunately, efforts to screen for the disease (e.g. DXA/DEXA or bone density scans) have helped doctors diagnose cases of osteoporosis before the disease progresses to the point of bone fracture.
The main treatment for osteoporosis is a class of drugs called bisphosphonates. Bisphosphonates block the cells that resorb bone (osteoclasts) to allow the cells that form new bone (osteoblasts) to catch up. While bisphosphonates are effective, many patients experience severe GI side effects from these drugs including reflux, esophagitis, and ulcers, and cannot take them.
In an effort to find new ways to treat osteoporosis and help patients who cannot tolerate bisphosphonates, researchers are exploring the possibility of using stem cells to treat the disease. Ideally, one would take stem cells from patients to help regrow bone. What has been unclear was whether a person with osteoporosis still has enough healthy stem cells to effectively regrow bone.
To test this, Dr. Jiang and colleagues collected stem cells from the fat tissue of patients with osteoporosis (i.e. adipose-derived stem cells). The researchers took these stem cells and encouraged them to grow and multiply for 14 days. After the stem cells had proliferated, they injected the cells into mice and studied the effects on bone growth. After 4 weeks, the researchers saw evidence on X-ray scans that adipose-derived stem cells caused new bone growth.
These results demonstrate that even patients with osteoporosis still possess stem cells that can be used to treat their own osteoporosis. While the stem cells need to be treated in a laboratory setting for 14 days, it is potentially possible to use a patient’s own stem cells to regrow bone and treat their osteoporosis.
The next phase of research will be to conduct a clinical trial to show test whether autologous stem cell treatment (injecting a patient with their own stem cells) can regrow bone in humans. While those clinical studies will be critical in determining whether this approach is practical and effective for patients, this laboratory research is very promising.
Contact us today!
Reference: Jiang M. et al. (2014). Bone formation in adipose-derived stem cells isolated from elderly patients with osteoporosis: a preliminary study. Cell Biology International. 2014 Jan;38(1):97-105.

by admin | Oct 25, 2019 | Adipose, Osteoarthritis, Stem Cell Research, Stem Cell Therapy
Osteoporosis is a disease in which bones become weak, brittle, and are prone to fracture. While osteoporosis is commonly considered a disease of low bone density, it is actually more complex and extensive than that. New bone is constantly formed and destroyed (resorbed) throughout life. In osteoporosis, however, the rate at which it is resorbed accelerates, while the rate at which it is formed slows down. In other words, bone is being destroyed faster than it can be formed. This process changes the size and shape of bones and alters its microarchitecture (i.e. the structure of bone on a microscopic level).
Without screening, most people will not know that they have osteoporosis until they have a bone fracture. Bones simply get weaker until some minor trauma causes one or more bones to break. Fortunately, efforts to screen for the disease (e.g. DXA/DEXA or bone density scans) have helped doctors diagnose cases of osteoporosis before the disease progresses to the point of bone fracture.
The main treatment for osteoporosis is a class of drugs called bisphosphonates. Bisphosphonates block the cells that resorb bone (osteoclasts) to allow the cells that form new bone (osteoblasts) to catch up. While bisphosphonates are effective, many patients experience severe GI side effects from these drugs including reflux, esophagitis, and ulcers, and cannot take them.
In an effort to find new ways to treat osteoporosis and help patients who cannot tolerate bisphosphonates, researchers are exploring the possibility of using stem cells to treat the disease. Ideally, one would take stem cells from patients, purify them, get the cells to multiply in the lab, and inject them back into patients with osteoporosis to help regrow bone. What has been unclear was whether a person with osteoporosis still has enough healthy stem cells to effectively regrow bone.
To test this, Dr. Jiang and colleagues collected stem cells from fat tissue of patients with osteoporosis (i.e. adipose-derived stem cells). The researchers took these stem cells and encouraged them to grow and multiply for 14 days. After the stem cells had proliferated, they injected the cells into mice and studied the effects on bone growth. After 4 weeks, the researchers saw evidence on X-ray scans that adipose-derived stem cells caused new bone growth.
These results demonstrate that even patients with osteoporosis still possess stem cells that can be used to treat their own osteoporosis. While the stem cells need to be treated in a laboratory setting for 14 days, it is potentially possible to use a patient’s own stem cells to regrow bone and treat their osteoporosis.
The next phase of research will be to conduct a clinical trial to show test whether autologous stem cell treatment (injecting a patient with their own stem cells) can regrow bone in humans. While those clinical studies will be critical in determining whether this approach is practical and effective for patients, this laboratory research is very promising.
Reference: Jiang, M. et al. (2014). Bone formation in adipose-derived stem cells isolated from elderly patients with osteoporosis: a preliminary study. Cell Biology International. 2014 Jan;38(1):97-105.

by admin | Oct 23, 2019 | Age Management, Stem Cell Research, Stem Cell Therapy
Autologous stem cell treatments offer several advantages over other forms of stem cell treatment. In autologous stem cell treatment, a patient’s own stem cells are retrieved, processed, and injected back into the patient’s body. There is no need for a stem cell donor, and the entire procedure can take place in the same medical office. Since the patient’s own cells are used for an autologous stem cell treatment, there is no risk of disease transmission from a donor (because there is no donor) and no risk of rejection (because they are the patient’s own stem cells).
Unfortunately, younger stem cells are better for regenerative medicine than older stem cells are. Moreover, older people have fewer stem cells that can be harvested than they did when they were younger. So while autologous stem cell treatment is still advantageous, it becomes more difficult to achieve as patients get older because their stem cells are fewer and less potent. Making matters worse, older stem cells compete against more youthful stem cells, making autologous stem cell treatments potentially even less effective in older patients.
Fortunately, stem cell researchers are coming up with ways to make the most out of the stem cells that older patients still have. They still take a sample of tissue, such as fat, and harvest the stem cells contained within it. However, instead of injecting all stem cells from the sample (both older and youthful stem cells), researchers select and use only youthful stem cells. Furthermore, they make the treatments even more effective by injecting other substances (e.g. extracellular matrix) that helps youthful stem cells survive, grow, and thrive.
To demonstrate the effectiveness of their approach, researchers collected mesenchymal stem cells from about a dozen older individuals aged 65 to 86 years old. They then assorted the stem cells into different groups, separating youthful from older stem cells. They then used special factors to help the youthful stem cells grow, increasing the numbers by an impressive 17,000 times. So while only 8% of stem cells produced by older individuals are “youthful,” this laboratory process increased those numbers to a point that they can be used for stem cell treatments—even stored for future use!
The next phase of the research will be to inject these youthful stem cells into older patients and assess their effectiveness. However, even these preliminary results are exciting, because they suggest that people of all ages can potentially benefit from autologous stem cell treatments, not just middle age and younger individuals.
Reference: Block, TJ et al. (2017). Restoring the quantity and quality of elderly human mesenchymal stem cells for autologous cell-based therapies. Stem Cell Research and Therapy. 2017 Oct 27;8(1):239.

by admin | Oct 18, 2019 | Adipose, Erectile Dysfunction, Stem Cell Research, Stem Cell Therapy
Prostate cancer is quite common among men in the United States. The main treatment options for prostate cancer include:
- External beam radiation – Radiation is applied to the prostate gland through the skin (noninvasive)
- Brachytherapy – Radioactive pellets the size of grains of rice are placed within the prostate gland (invasive)
- Radical prostatectomy – The entire prostate gland and some surrounding tissue is removed
About one-quarter of all men with prostate cancer ultimately choose to have a radical prostatectomy. Unfortunately, this procedure often leaves men with chronic problems afterward, such as urinary incontinence (i.e., the inability to hold or control urine) and erectile dysfunction (i.e., the inability to achieve and maintain a penile erection suitable for sexual intercourse). Almost 90% of men who undergo radical prostatectomy to treat prostate cancer develop erectile dysfunction. Drugs and penile injections are not always effective in treating this type of erectile dysfunction. Consequently, as many as three-quarters of men must live with permanent erectile dysfunction. While prostate cancer is essentially cured after radical prostatectomy, affected men have substantially worse quality of life, which also negatively affects their sexual partners.
In an effort to combat this difficult problem, researchers conducted a Phase 1 clinical trial in which they took stem cells from the patient’s own fat tissue (autologous stem cells), purified them, and injected them into the penile tissue of radical prostatectomy patients with erectile dysfunction. Eight of the 17 men who volunteered for the clinical trial regained erectile function and were able to engage in sexual intercourse after just one stem cell injection.
Importantly, stem cell treatment was only effective for men who had not developed urinary incontinence. Eight of 11 men who still could control their urine after radical prostatectomy regained their ability to achieve and maintain erections. Conversely, no man with urinary incontinence after radical prostatectomy had erectile function restored.
The researchers noted that the stem cell treatment was very well tolerated by all men, and described the procedure as safe.
While larger clinical trials are needed to confirm these results, autologous stem cells taken from a patient’s own fat tissue were able to restore erectile function in most of the men treated. This research suggests that men who do not lose urinary function may benefit from this procedure. On the other hand, men who become incontinent after radical prostatectomy may not benefit from this particular stem cell therapy. Randomized, placebo-controlled clinical trials will help clarify this issue. In the meantime, these results are encouraging news to thousands of men who suffer from permanent erectile dysfunction as a result of their radical prostatectomies.
Reference: Haahr, MK et al. (2016). Safety and Potential Effect of a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. EBioMedicine. 2016 Jan 19;5:204-10.




 St. Petersburg, Florida
St. Petersburg, Florida
