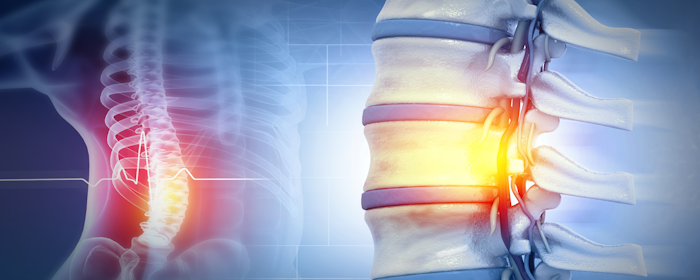
Understanding Spinal Cord Injuries (SCI)
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified PhysicianLast Updated: October 2025 What Is a Spinal Cord Injury? A spinal cord injury (SCI) occurs when trauma or disease disrupts the communication between the brain and the rest of the body.This damage can result from accidents, falls, infections, or tumors, and depending on where the injury…