
by admin | Jan 4, 2019 | Stem Cell Research, Stem Cell Therapy, Studies
Spinal cord injury can be one of the most devastating
injuries. Long neurons that extend from the brain down the spinal cord are
severed and scarred. In most cases, this damage can never be repaired. If
patients survive an injury to the spinal cord, they can be permanently
paralyzed. Researchers have attempted to use high-dose steroids and surgery to
preserve the spinal cord, but these approaches are either controversial or
largely ineffective.
Ideally, one would create an environment in which nerve
cells in the spinal cord could regrow and take up their old tasks of sensation
and movement. One of the most promising approaches to do just this is stem cell
transplantation.
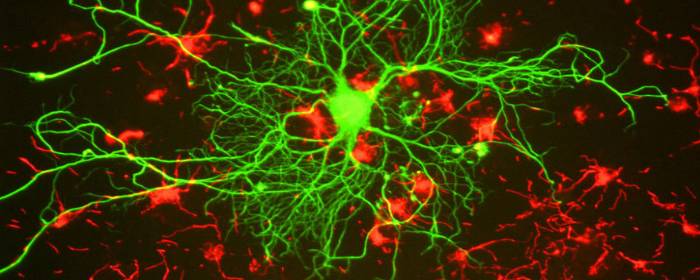
To test this concept, researchers used
stem cells derived from human placenta-derived mesenchymal
stem cell tissue (not embryonic stem cells) to form neural stem cells in
the laboratory. These neural stem cells have the ability to become neuron-like
cells, similar to those found in the spinal cord. The researchers then used
these stem cells to treat rats that had experimental spinal cord injury. The
results were impressive.
Rats treated with neural stem cells regained the partial
ability to use their hindlimbs within one week after treatment. By three weeks
after treatment, injured rats had regained substantial use of their hindlimbs.
The researchers confirmed that this improvement was due to neuron growth by
using various specialized tests (e.g. electrophysiology, histopathology). Rats
that did not receive stem cells did not regain substantial use of their
hindlimbs at any point in the study.
This work is particularly exciting because it shows that
stem cells can restore movement to animals who were paralyzed after spinal cord
injury. Moreover, the researchers used human stem cells derived from placenta,
which suggests that this effect could be useful in human spinal cord injury
patients (perhaps even more so than in rats). While additional work is needed,
these results offer hope to those who may one day develop severe spinal cord
injury.
Reference:
Zhi et al. (2014). Transplantation of placenta-derived
mesenchymal stem cell-induced neural stem cells to treat spinal cord injury.
Neural Regen Research, 9(24): 2197–2204.

by admin | Dec 29, 2018 | Mesenchymal Stem Cells, Osteoarthritis, Stem Cell Therapy
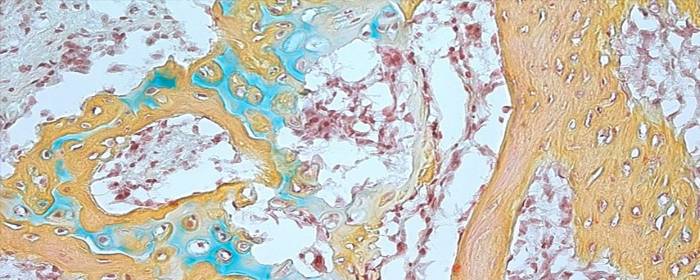
Most large joints of the body contain cartilage, a substance that is softer and more flexible than bone. Because of its softness and flexibility, cartilage is well-suited to protect the bones as they move across one another. Unfortunately, this softness and flexibility also makes cartilage prone to injury and erosion. In patients with osteoarthritis, forexample, cartilage breaks down to the point that bone rubs against bone,causing pain and disability. Certain injuries can damage the cartilage (i.e.osteochondral lesion), which can essentially have the same effect.
Once the cartilage of joints has become damaged, there is
little that can be done to fix it. Patients may receive steroid injections into
the joint to reduce inflammation, and may rely on pain medications to relieve
the pain and swelling. Short of joint replacement therapy, no treatments can
reverse cartilage damage once it has occurred.
Fortunately, mesenchymal stem cells may soon be able to reverse cartilage defects that arise from osteochondral lesions and osteoarthritis. Wakitani and colleagues took samples of patients’ bone marrow, which contains mesenchymal stem cells. They then used various laboratory techniques to increase the number of stem cells in the sample. Four weekslater, the researchers then reinjected the concentrated stem cells back intothe same patient using their own source of stem cells. The Wakitani groupshowed that stem cell transplantation improved the patient’s clinical symptoms bysix months, a benefit that continued for two years on average. Samples takenfrom the patients 12 months later showed that the damaged cartilage had beenrepaired. In other work, Centeno and co-authors showed that bone marrow-derived mesenchymal stemcells could increase the volume of cartilage, reduce pain, and increase rangeof motion 24 weeks after stem cell transplantation.
Research continues to determine which stem cells are most useful, how many stem cells should be injected, how many injections need to be administered, and how should those stem cells be prepared before they are injected? Nonetheless, certain groups are making great strides in this area. In fact, the recent discovery of human skeletal stem cells promises to accelerate stem cell research into treating disorders of bone and cartilage.
Reference
Schmitt et al. (2012). Application of Stem Cells in Orthopedics. Stem Cells International. 2012: 394962

by admin | Dec 27, 2018 | Stem Cell Research, Stem Cell Therapy
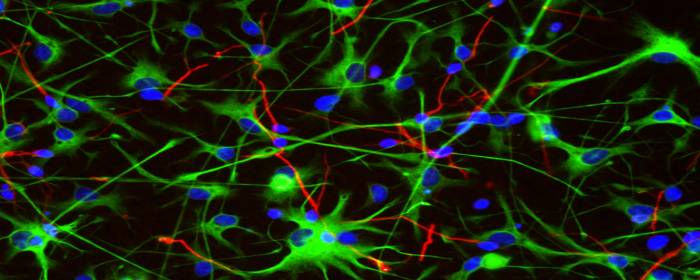
A number of different stem cell types have been shown to exert significant therapeutic effects when transplanted into the central nervous system. These cells include non-hematopoietic stem cells such as mesenchymal stem cells and neural/progenitor stem cells and carry out their effects by secreting what are known as neurotrophic paracrine factors, whichhelp to control the immune system.
In recent years, it has been suggested that rather than requiring the injection of stem cells, brain injury repair may be achieved by injecting the molecules that stem cells tend to secrete – known as secretome. The stem cell secretome includes growth factors as well as cytokines and chemokines. Investigators have begun to explore whether delivering these substances, rather than stem cells, could offer a more efficient means to therapy.
The rationale is that by delivering these substances directly, it should be possible to stimulate the proliferation of progenitor cells in the central nervous system and therefore instigate repair. However, initial studies have shown that the infusion of individual cytokines does not have the expected effect. According to the authors of a review published in Biochimie, it may be that multiple substances will need to be simultaneously infused in pre-tested concentrations so that they can act synergistically to optimize therapeutic effects.
Clinical trials are underway to determine the safety to patients of the secretome approach and to identify any relevant risks so that potential risks can be weighed against potential benefits of this type of therapeutic approach. There is also research on a wide variety of topics that will need clarification if effective stem cell secretome therapies are to be developed for brain repair. These topics include clarifying aspects of tissue transport and determining the mechanisms by which secretomes confer their benefits.
Reference: Drago, D. (2014). The stem cell secretome and its
role in brain repair. Biochimie, 95(12),
2271-2285.

by admin | Dec 12, 2018 | Stem Cell Therapy
Stem cell therapy is used for a broad range of applications, including the treatment of injuries and chronic conditions. Before undergoing this form of therapy, many patients are naturally inclined to explore any possibilities which could enhance the effectiveness of treatment. One option which is sometimes posed to patients is voluntary fasting – but is there really any benefit to fasting prior to stem cell treatment?
What the Research Says
In May of 2018, MIT biologists announced that they’d made a groundbreaking discovery: according to their research, it appeared that fasting could boost stem cells’ regenerative capacity. In an animal study, fasting spurred cells to break down fatty acids instead of glucose, which stimulates stem cells to become more regenerative.
Yet, the evidence only showed the metabolic switch taking place in the intestinal stem cells. After mice fasted for 24 hours, the researchers removed intestinal stem cells and grew them, finding that the fasting doubled the cells’ regenerative capacity.
Unfortunately, while this finding could hold value for patients recovering from gastrointestinal infections or other conditions affecting the intestine, as of yet, there is no concrete evidence which suggests it could benefit patients receiving stem cell therapy for other conditions. For instance, someone who is undergoing stem cell therapy to treat a musculoskeletal injury may likely yield no benefit from fasting, as the enhanced regenerative effects have only been observed in intestinal cells.
Further Studies Are Needed
Aside from the study’s limited scope, the research leader himself also indicated that the findings are still too narrow for drawing concrete conclusions. When interviewed for a publication in Medium, senior author of the study and assistant professor of biology, Omer Yilmaz, said that while stem cells do indeed use fat for energy to improve function, “the next step is to work to understand why that is.” He also added that “with these types of interventions, there’s never one simple answer.”
For now, there appears to be too much uncertainty to recommend fasting prior to stem cell therapy. Because these findings have not been observed in any humans, and those that have been observed were concentrated to intestinal cells, anyone who is receiving stem cell therapy can consider that eating beforehand is possibly unlikely to play any role in altering the results of their treatment.

by admin | Dec 3, 2018 | Osteoarthritis, Stem Cell Research, Studies
The human skeleton is made up of bone, cartilage, fat, nerves, blood vessels, and bone marrow. While the skeleton is usually strong and vibrant in youth, it changes considerably with age. Many people, especially women, experience demineralization of bone called osteoporosis. Most of us will suffer from painful, stiff, arthritic joints either from osteoarthritis or rheumatoid arthritis or both. While some of the diseases of bone and joints have specific treatments, none of them helps to restore bone and joints to their younger state. If one could reintroduce skeletal stem cells into the body, that could all change. Excitingly, researchers have recently isolated human skeletal stem cells from bone and other tissues.
At first glance, this breakthrough may not seem so surprising. One might wonder: didn’t we already have stem cells that form bone and cartilage? The answer is yes, but with an important caveat. Before researchers recently isolated human skeletal stem cells, the only stem cells that could be used to produce bone and cartilage were rather unpredictable. In addition to bone and cartilage, the mesenchymal stem cells that have been long used to form these tissues could also produce fat, muscle, fiberglass, blood vessel cells, and other tissues. In other words, the stem cells were broadly multipotent and, by extension, could not easily be used for a specific purpose, like mending bone or repairing an arthritic joint. That is why the recent discovery of these particular skeletal stem cells is so important.
The researchers isolated skeletal stem cells from various human tissues, mainly bone. They then used the skeletal stem cells to regrow bone and/or cartilage. Not only did the stem cells produce bone and cartilage in the first animal they tested, but they could retrieve stem cells from that animal and then cause bone to regrow in a second animal. This means that the skeletal stem cells have the capability of reproducing themselves.
The same researchers also discovered that when a skeleton is injured, such as in a bone fracture, the number of skeletal stem cells in that area increases dramatically. This makes sense since these cells are used to repair and regrow bone. It is also a promising result because it suggests that stem cells could be used to accelerate bone and joint healing in humans.
Scientists not directly involved in this research heralded this finding as “an extremely important advance.” However, they also acknowledge that more work needs to be done before skeletal stem cells can be routinely used in patients with orthopedic conditions. Nevertheless, these results are an exciting development in the field of stem cell research and orthopedics.
Reference: https://www.sciencenews.org/article/humans-have-skeletal-stem-cells-help-bones-and-cartilage-grow



 St. Petersburg, Florida
St. Petersburg, Florida
