
by admin | Sep 7, 2018 | Stem Cell Therapy
Multipotent stem cells have the ability to turn into a number of different cells in the body, making them one of the most versatile solutions in regenerative medicine. They are also characterized by their capacity for self-renewal. Here, we take a look at their current applications, as well as their benefits.
What Makes Multipotent Stem Cells Unique?
To understand the distinguishing features of multipotent stem cells, we must first look at the different types of stem cells. There are three main classifications for the varying degrees of stem cell flexibility:
- Totipotent: These cells can turn into any cell in the body and are only found within the first couple of cell divisions following the fertilization of a female egg by a male sperm.
- Pluripotent: During embryonic development, totipotent cells specialize into pluripotent cells. They can give rise to all cells in the human body but aren’t quite as flexible as totipotent cells.
- Multipotent: Finally, pluripotent stem cells specialize into multipotent stem cells, which have been found in cord blood, cord tissue, adipose tissue, cardiac cells, bone marrow, and mesenchymal stem cells (MSCs).
What Are Multipotent Stem Cells Used for?
Not only are multipotent stem cells able to renew themselves almost indefinitely, their ability to become any other cell makes them a powerful agent in treating patients with tissue damage. From knees to other joints and even the gastrointestinal tract, there are many sites in the body where compromised tissue can benefit tremendously from stem cells. They can even help arthritis sufferers and individuals with tendonitis. Because stem cells can also replenish dying or damaged tissue of specialized cell types, multipotent stem cells can also benefit individuals with chronic illnesses such as COPD, multiple sclerosis (MS), and Parkinson’s disease.
What Are the Benefits of Multipotent Stem Cells?
Multipotent stem cells are advantageous because they can be sourced from a number of locations, including the Wharton’s Jelly which lines umbilical cord vessels, as well as fat tissue (adipose stem cells) and bone marrow aspirate. These cells can then be delivered via non-invasive regenerative therapy to replace damaged cells with new ones, which have the ability to help increase energy and control symptoms in chronic conditions. The treatment can also potentially spur healthy tissue development in musculoskeletal injuries, and when injected directly into the joint, it has the potential to promote healing of ligaments, tendons, and cartilage to help return functionality and in some cases could delay the need for joint replacement.

by admin | Sep 5, 2018 | Hyperbaric Oxygen Therapy, Stem Cell Research, Stem Cell Therapy, Studies, Traumatic Brain Injury
Traumatic brain injury (TBI) is one of the most common causes of disability in the United States, affecting over 13 million citizens. Traumatic brain injury is responsible for over 2 million emergency department visits, over a quarter of 1 million hospitalizations, and nearly 60,000 deaths each year.
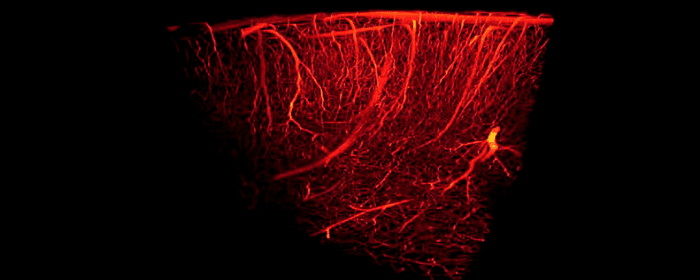
Traumatic brain injury harms brain tissue in two phases. The first phase of injury occurs at the time of the traumatic incident. This initial injury may cause small or large areas of the brain to bleed. It may also shear (stretch/tear) nerve cells, making them dysfunctional. The second phase occurs hours or days after the initial injury. The brain is subjected to ongoing damage because of inflammation, cell death, and injury to blood vessels. Many people with TBI are left with lifelong problems with thinking, memory, and behavior.
In both of these phases of injury, one major way to help prevent long-term brain damage is by maintaining adequate blood flow to brain tissue. Unfortunately, once the damage has occurred, it can be a challenge to reverse the damage. Patients usually must endure months or years of physical and occupational therapy to regain what was lost. Moreover, patients often need substantial amounts of psychiatric and psychological support to treat mental health problems.
Fortunately, researchers are using hyperbaric oxygen therapy (HBOT) to improve blood flow to the brain in patients with traumatic brain injury. Hyperbaric oxygen therapy provides patients with pure oxygen (100%) at slightly higher pressures than they would experience normally. It is been used for hundreds of years to treat scuba divers who suffered “the bends” or decompression sickness; however, researchers are finding that hyperbaric oxygen therapy is a “coveted neurotherapeutic method for brain repair.”
To study the effects of hyperbaric oxygen therapy, researchers selected 10 people who had suffered mild traumatic brain injury in the previous 7 to 13 years. Patients all had brain damage that interfered with attention, memory, and thinking abilities.
Even though patients had sustained traumatic brain injury and brain damage a decade earlier, hyperbaric oxygen therapy was able to improve blood flow in the brain. Likewise, the amount of blood detected within the brain significantly increased, suggesting that hyperbaric oxygen therapy actually caused blood vessels in the brain to grow and multiply. Just as impressively, patients with chronic brain damage performed better on tests of cognition (i.e. thinking). They were able to process information more quickly, they had better motor function, and they were able to take in and process information about the world around them more efficiently.
Because people with traumatic brain damage have limited treatment options to improve their situations, these results are incredibly exciting. This was a study on 10 patients and more studies on larger numbers are still needed to build on these findings. Nonetheless, these results are quite encouraging for people with traumatic brain injury and their loved ones.

by admin | Aug 28, 2018 | Stem Cell Research, Stem Cell Therapy
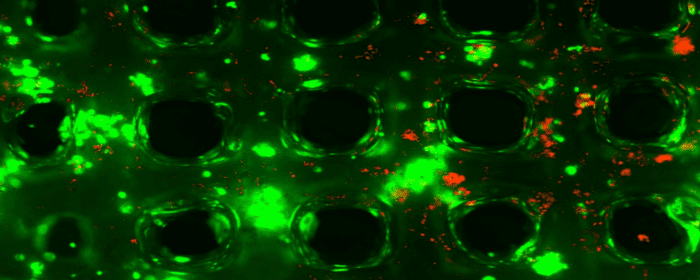
The evidence for the promise of mesenchymal stem cells in regenerative medicine has been growing for several years. With new sources regularly emerging, stem cells can come from a large variety of sources. Postnatal mesenchymal stem cells appear to have the most promise in regeneration. A new review has addressed how mesenchymal stem cells can be used with innovative scaffolding engineering approaches to improve techniques in regenerative medicine.
Mesenchymal stem cells are, on their own, good candidates for regeneration because of a number of characteristic features. For instance, they can differentiate into many different types of cells. Osteoblasts and chondroblasts are two cell types that mesenchymal stem cells differentiate into and that can be supported in bone regeneration by 3D-printed biomaterials like scaffolds.
Mesenchymal stem cells also can have beneficial impacts on the immune system. Unlike with other stem cell types, the severe immune reactions that may occur with the transplantation of foreign materials into the body can often be avoided with the use of mesenchymal stem cells, making them a safe option in regenerative medicine.
The current review addresses the ways in which bone regeneration can be optimized through the use of mesenchymal stem cells and scaffold engineering and how new concepts in bioengineering may be able to improve regenerative medicine in combination with mesenchymal stem cell approaches. Future research will need to focus on how we can customize regenerative approaches using what we know about mesenchymal stem cells and the most cutting-edge innovations in bioengineering.

by admin | Aug 27, 2018 | Adipose, Stem Cell Research, Stem Cell Therapy
Regenerative medicine is a field of research concerned with the process of replacing diseased, dying, or dead cells with the intent of restoring structure and function. In its most basic form, regenerative medicine seeks to regrow cells that were lost or damaged due to injury or condition. Examples of regenerative medicine applications include restoring heart cells after a heart attack, repairing brain cells in Alzheimer’s disease or after stroke, or regenerating T-cells in HIV/AIDS. The potential applications of regenerative medicine are virtually limitless.
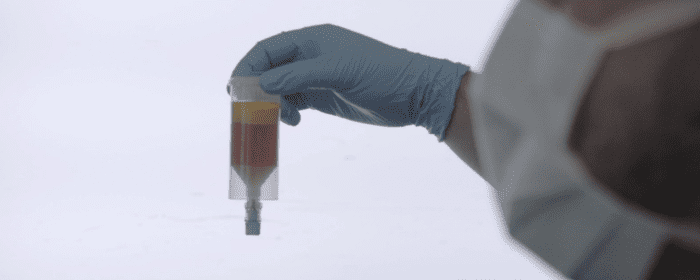
Adipose-derived stem cells hold great promise in the field of regenerative medicine. The stem cells are multipotent, which means they can become any number of cell types. For example, adipose-derived stem cells can become osteocytes (bone cells), neural cells (nerve cells), vascular endothelial cells (cells that make up blood vessels), cardiomyocytes (heart muscle cells), pancreatic β-cells (cells that produce insulin), and hepatocytes (liver cells).
Adipose- or fat-derived stem cells have one obvious advantage over bone marrow cells: they are much easier to obtain. Bone marrow stem cells require an uncomfortable/painful procedure to extract them from the center of the bone. Fat-derived stem cells, on the other hand, can be taken from fat pockets in any number of places just under the skin. This essentially combines a sort of liposuction with stem cell transplantation.
Adipose-derived stem cells are the subject of nearly 200 clinical trials worldwide. Even now, fat-derived stem cells are proving useful in several clinical conditions. Adipose-derived stem cells were shown to help people after they suffered from a heart attack, by reducing the size of the damaged heart and helping to restore heart function.
Another advantage of adipose-derived stem cells is that they present possess a tri-germ lineage differentiation potential, meaning they can differentiate into all three germ layers. In other words, they have the remarkable potential to become virtually any cell in the body. This means they can be applied to more than one disease state. In neurodegenerative diseases, such as post-stroke, adipose-derived stem cells could be used to create nerve cells (neurons) and the other main type of brain cell, called glia. Both cell types are destroyed during a stroke, and both are important for proper brain function.
As more results are published from dozens of clinical trials, we will get a clearer picture of the therapeutic potential of adipose-derived stem cells. Indeed, the future of regenerative medicine is very bright.

by admin | Aug 21, 2018 | Stem Cell Therapy, Wharton's Jelly
Mesenchymal stem cells have been showing promise in the treatment of a variety of diseases and injuries. These cells are derived from different tissue types, and it appears that where the stem cells come from is indicative of how they function and how appropriate they are for use in different applications. Bone marrow-derived mesenchymal stem cells have been deeply studied and are often considered a go-to for stem cell research and clinical use.
However, there are several limitations that bone marrow-derived mesenchymal stem cells pose, particularly from a practicality standpoint, and thus, researchers have begun to try to understand how other types of stem cells may achieve similar or better results than those from the bone marrow. A recent review, published in Act Histochemical, compiled comprehensive data on the biological properties associated with a specific type of mesenchymal stem cell called Wharton’s Jelly-derived mesenchymal stem cells.
These stem cells, which come from the umbilical cord, are able to differentiate into mature cells that make up several different types of tissues and can even turn into non-mesenchymal cells, such as neurons, or brain cells. They are useful in that they spontaneously move to sites of injury or inflammation and may, therefore, be able to help restore tissue and normal functioning. They are also unlikely to instigate adverse immune system reactions.
While it is advantageous that bone marrow-derived mesenchymal stem cells have been studied extensively and therefore are associated with broad knowledge of therapeutic applicability, the cells are difficult to isolate and use. In contract, cells from the umbilical cord matrix, or Wharton’s jelly, are easy to isolate and also appear to be good candidates for therapeutic intervention. Future research should therefore look more closely at how Wharton’s jelly-derived mesenchymal stem cells can be used to treat disease and injury. As noted by the authors of this review, there are specifically dysfunctions of the central and peripheral nervous system that these stem cells may be able to address.

 St. Petersburg, Florida
St. Petersburg, Florida
