
by admin | Dec 3, 2018 | Osteoarthritis, Stem Cell Research, Studies
The human skeleton is made up of bone, cartilage, fat, nerves, blood vessels, and bone marrow. While the skeleton is usually strong and vibrant in youth, it changes considerably with age. Many people, especially women, experience demineralization of bone called osteoporosis. Most of us will suffer from painful, stiff, arthritic joints either from osteoarthritis or rheumatoid arthritis or both. While some of the diseases of bone and joints have specific treatments, none of them helps to restore bone and joints to their younger state. If one could reintroduce skeletal stem cells into the body, that could all change. Excitingly, researchers have recently isolated human skeletal stem cells from bone and other tissues.
At first glance, this breakthrough may not seem so surprising. One might wonder: didn’t we already have stem cells that form bone and cartilage? The answer is yes, but with an important caveat. Before researchers recently isolated human skeletal stem cells, the only stem cells that could be used to produce bone and cartilage were rather unpredictable. In addition to bone and cartilage, the mesenchymal stem cells that have been long used to form these tissues could also produce fat, muscle, fiberglass, blood vessel cells, and other tissues. In other words, the stem cells were broadly multipotent and, by extension, could not easily be used for a specific purpose, like mending bone or repairing an arthritic joint. That is why the recent discovery of these particular skeletal stem cells is so important.
The researchers isolated skeletal stem cells from various human tissues, mainly bone. They then used the skeletal stem cells to regrow bone and/or cartilage. Not only did the stem cells produce bone and cartilage in the first animal they tested, but they could retrieve stem cells from that animal and then cause bone to regrow in a second animal. This means that the skeletal stem cells have the capability of reproducing themselves.
The same researchers also discovered that when a skeleton is injured, such as in a bone fracture, the number of skeletal stem cells in that area increases dramatically. This makes sense since these cells are used to repair and regrow bone. It is also a promising result because it suggests that stem cells could be used to accelerate bone and joint healing in humans.
Scientists not directly involved in this research heralded this finding as “an extremely important advance.” However, they also acknowledge that more work needs to be done before skeletal stem cells can be routinely used in patients with orthopedic conditions. Nevertheless, these results are an exciting development in the field of stem cell research and orthopedics.
Reference: https://www.sciencenews.org/article/humans-have-skeletal-stem-cells-help-bones-and-cartilage-grow

by admin | Nov 19, 2018 | Adipose, Osteoarthritis, Stem Cell Research, Stem Cell Therapy
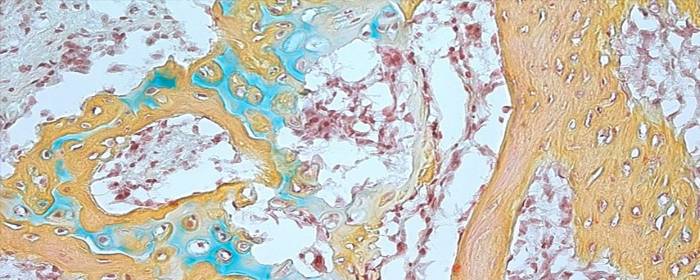
Bone generally develops via one of two distinct mechanisms: intramembranous ossification and endochondral ossification. In the former case, mesenchymal progenitor cells directly differentiate into osteoblasts that form bone. In the latter case, the mesenchymal progenitor cells first create a matrix of cartilage that then acts as a template to enable the remodeling or development of bone tissue. This process of endochondral ossification is the predominant way that bone is generating during the healing process after bones are broken and fractures are endured. Using stem cells to facilitate this process can, therefore, be beneficial in non-healing bone fractures.
A new study published in Acta Biomaterialia has proposed that adipose tissue can be used in bone generation as a scaffold on which adipose mesenchymal stem cells can expand and allow for endochondral ossification. The researchers showed how adipose tissue could be used in this way, through what they termed Adiscaf, to successfully generate cartilage tissue and eventually bone tissue formation. The bone tissue that formed through this process contained bone marrow elements, further demonstrating the bone’s integrity and the promise of this procedure.
Compared to other strategies for building scaffolding, this strategy appeared successful because by using adipose tissue, the adipose stem cells were exposed to their native environment and therefore likely maintained functions they otherwise may not have. Not only will these findings help to solidify our understanding of how to nurture stem cells and enable them to differentiate in ways that can be therapeutically applicable, but they also specifically show how adipose tissue may be able to be used to generate a bone organ through endochondral ossification. Future research will likely help to clarify how these findings can be applied to patients to improve bone healing.

by admin | Sep 13, 2018 | Stem Cell Research, Stem Cell Therapy, Studies
Patients usually recover from bone fractures with the right treatment, but sometimes the bone fails to heal because new tissue does not form and connect the broken pieces properly. Delayed union refers to cases where the bone takes longer than usual to heal, and nonunion refers to cases where the bone does not heal. In approximately 5 to 10 percent of cases of a fractured bone, delayed union or nonunion occurs. These conditions are associated with long-term pain and discomfort, and though can be addressed through surgical treatments, these interventions do not always lead to long-term healing.
In recent years, researchers have begun exploring the potential for mesenchymal stem cells to help address these important challenges of delayed union and nonunion. A review of the potential for these stem cells to help in these cases where fractures do not properly heal was recently published in the Journal of Biomedical Materials Research.
Mesenchymal stem cells are helpful in bone healing because they differentiate well and can differentiate into different cell lineages that are all important for bone formation, growth, and maintenance. These cell types include chondrocytes, osteoblasts, myoblasts, and adipocytes.
According to the authors of the review, mesenchymal stem cells can be used in conjunction with extracellular matrix scaffolds and biological adjuvants that promote growth, differentiation, and blood vessel formation, to help in the bone healing process when the delayed union or nonunion occurs. Future research will help to determine the best ways that mesenchymal stem cells can be used in combination with bioengineering strategies to help patients whose bone fractures do not heal or do not heal properly.

by admin | Jul 25, 2018 | Bone Marrow, Health Awareness, Stem Cell Research, Stem Cell Therapy
Stem cells derived from bone marrow, or hematopoietic stem cells, are a topic of significant debate in the medical community. While they have exhibited significant potential for benefiting people with both cancerous and noncancerous diseases including immune deficiencies, not all methods for administering bone marrow are created equal. While intra-articular injections of bone marrow are more common and considered safer, intravenous methods pose serious risks, which are explored here.
Intra-articular injections involve injecting bone marrow directly into the compromised joint, whereas intravenous methods entail infusing bone marrow stem cells into the body through the veins. Intra-articular injections have shown promise in treating conditions such as osteoarthritis (OA) in joints such as the knee and has proven to achieve pain relief for moderate-to-severe cases of osteoarthritis.
Intra-articular treatments are localized, so the injected bone marrow is already in its target location upon being administered. According to research, this form of therapy is generally considered to be safe. In intravenous bone marrow transplants, however, there are serious risks associated with treatment. Bacterial infections are common, while viral and fungal infections can also occur and cause life-threatening conditions, such as organ failure.
Risk factors for developing any complication associated with intravenous bone marrow transplantations vary based on a number of factors, including the patient’s age, genetics, and type of disease being treated. With that said, due to its limited risks, intra-articular bone marrow methods appear to be the safest form of treatment currently available. Although each patient will need to discuss risk factors alongside potential benefits with his or her physician, oftentimes the risks appear to outweigh the potential benefits.
There are alternative therapies with fewer potential side effects which may be explored such as Adipose and Umbilical Cord-derived stem cells. These regenerative medicine treatments not only can treat osteoarthritis and sports-related injury conditions, but have also shown positive results in treating neurological conditions such as Multiple Sclerosis, Parkinson’s disease, Post-Stroke, and Traumatic Brain Injuries (TBI).

by admin | Sep 27, 2017 | Osteoarthritis
In a review published in Stem Cell Research & Therapy, Gupta et al. describe the latest advances in the use of bone marrow derived stem cells to treat osteoarthritis. These cells are promising because of their ability to treat the degeneration of cartilage that occurs in the disease. When connective tissue degenerates, natural regeneration is highly limited because there is not a strong presence of vasculature within that tissue. Thus, interventions to deal with the effects of osteoarthritis are needed.
Historically, non-stem cell treatments have been used in attempts to treat cartilage degeneration. Physical therapy, pharmaceuticals, and surgical interventions have all been largely employed. For mild cases of osteoarthritis, combinations of physical therapy and pharmaceuticals have been used to manage pain and minimize inflammation. Unfortunately, because the disease is progressive, this type of approach is only effective in the short-term.
Eventually, steroids or hyaluronic acid are generally used to treat osteoarthritis. The impact of these more aggressive treatments, however, is debated and does not appear to be consistent across patient populations. Once osteoarthritis reaches the advanced stage, joint replacement is the only option for relief.
The use of cell-based therapies to treat osteoarthritis is not a new idea. Cultured autologous chondrocytes have been shown to successfully treat cartilage degeneration for over 15 years. The downsides to this approach are that it is invasive, the positive effects are likely temporary, and there has not been sufficient research conducted to fully understand how well the technique works and how to optimize it.
Bone marrow derived stem cells have the potential to carry the same success rate as the cell-based therapies that have long been used to treat osteoarthritis while also overcoming the limitations of those therapies. There are several advantages of the application of bone marrow derived stem cells in the treatment of cartilage degeneration.
First, these particular cells can be easily isolated. Second, they can significantly expand in culture before being used therapeutically. Third, they have modulatory properties that enable them to reduce inflammation, which is a critical factor in cartilage degeneration. Finally, they secrete factors that have the potential to both prevent further degeneration and facilitate regeneration.
Given the number of reasons that bone derived stem cells should theoretically improve upon current methods for treating the cartilage degeneration that occurs in osteoarthritis, more research will likely be conducted to decipher whether these cells do indeed provide benefits that other treatment options do not. In the case that these cells continue to appear promising for osteoarthritis treatment, research will likely also aim at determining the best protocols for using these cells to ensure the best outcomes for osteoarthritis patients.
To find out more about the new alternative way to manage the symptoms of Osteoarthritis, click here.
Reference:
Gupta, PK, Das, AK, Chullikana, A, & Majumdar, A. (2012). Mesenchymal stem cells for cartilage repair in osteoarthritis. Stem Cell Research & Therapy, 3, 25-34.



 St. Petersburg, Florida
St. Petersburg, Florida
