
by admin | Feb 1, 2019 | Adipose, Exosomes, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Studies, Umbilical Stem Cell
Most organs of the body recover from injury by generating new, healthy cells. Not every organ of the body has the same ability to form new cells, however. The skin is an example of an organ that has an amazing ability to regenerate. Liver and lung also have the ability to form new cells, but not as dramatically as skin. Kidney and heart have even less ability to repair and regenerate. On the opposite end of the spectrum from the skin is the brain, which has very little capacity to regenerate once it has been damaged or destroyed. All of these organ systems, especially those that are relatively unable to repair themselves, could theoretically benefit from stem cells.
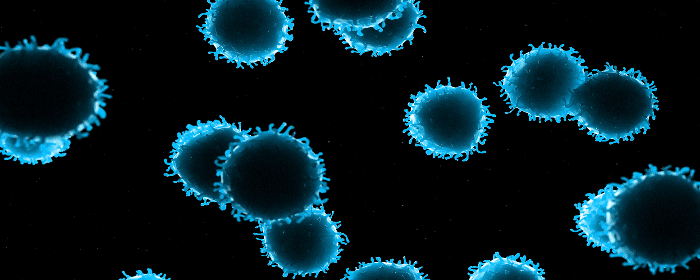
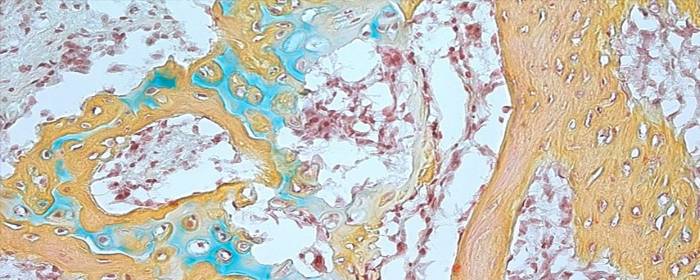
Mesenchymal stem cells, also known as stromal cells, are multipotent stem cells derived from bone marrow, umbilical cord, placenta, or adipose (fat) tissue. These cells can become the cells that make up bone, cartilage, fat, heart, blood vessels, and even brain. Mesenchymal stem cells have shown a remarkable ability to help the body to produce new cells. Researchers are now realizing that the substances stem cells release may be more important than any new cells they may become. In other words, stem cells can directly become new healthy cells to a certain degree, but they can also release substances that dramatically increase the number of new, healthy cells.
Mesenchymal stromal stem cells release small packets called exosomes. These exosomes are filled with various substances that promote cell and tissue growth. Some of the most interesting and potentially useful substances are cytokines and micro RNA. Cytokines are the traffic cops of cellular repair, signaling certain events to take place while stopping others. Having the right cytokines in a particular area is critical for new tissue growth. The micro RNA released by stem cell exosomes is potentially even more exciting than cytokines. These tiny bits of RNA can directly affect how healthy and diseased cells behave. Micro RNA has a powerful ability to control the biological machinery inside of cells.
Exosomes exhibit a wide array of biological effects that promote the repair and growth of damaged and diseased organs. They promote the growth of skin cells and help wounds heal. Exosomes can reduce lung swelling and inflammation and even help the lung tissue heal itself (i.e. reduced pulmonary hypertension, decrease ventricular hypertrophy, and improve lung vascular remodeling). These small packets released by stem cells help prevent liver cells from dying (i.e. prevents apoptosis), promote liver cell regeneration, and slow down liver cirrhosis (i.e. fibrosis). Exosomes can also help protect the kidneys during acute injury and reduce the damage that occurs during a heart attack.
Several clinical trials are underway designed to allow these exciting developments to be used to treat patients. As the researchers state, “Extensive research and clinical trials are currently underway for the use of MSCs as regenerative agents in many diseases including spinal cord injury, multiple sclerosis, Alzheimer’s disease, liver cirrhosis and hepatitis, osteoarthritis, myocardial infarction, kidney disease, inflammatory bowel disease, diabetes mellitus, knee cartilage injuries, organ transplantation, and graft-versus-host disease.” We can reasonably expect that exosomes will be used to treat at least some of these conditions in the very near future.
Reference: Rani al. (2015). Mesenchymal Stem Cell-derived Extracellular Vesicles: Toward Cell-free Therapeutic Applications. Molecular Therapy. 2015 May; 23(5): 812–823.

by admin | Jan 15, 2019 | Exosomes, Mesenchymal Stem Cells, Stem Cell Research, Studies
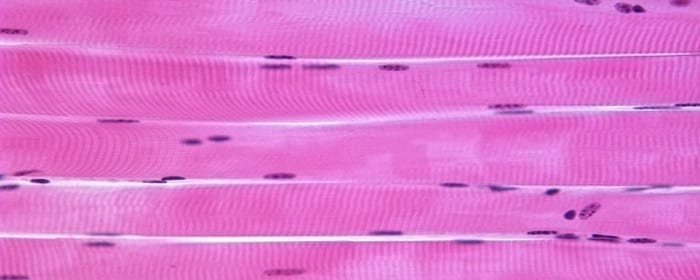
Muscle health and strength is an important determinant of a person’s ability to function in daily life. One of the major determinants of healthy aging is how well people retain their muscle mass. The more that skeletal muscle declines, the more likely someone would not be able to care for themselves independently. Injury to muscles whether through trauma, burns, or toxins can greatly interfere with a person’s ability to perform activities of daily living. While muscle cells have a limited ability to regenerate themselves, quite often, patients never regain their former strength and level of function after serious injury.
Stem cells would seem to be ideally suited to help in this regard. Since stem cells have the potential to become muscle cells, one could imagine infusing stem cells into an area of muscle damage or injury to restore overall muscle function. While this makes sense intuitively, it may not be the case. Stem cells, for example, form new muscle cells, but they do not form cells that participate in muscle function. And yet, stem cells are able to help muscles regrow into functional skeletal muscles.
How could stem cells promote skeletal muscle regeneration without becoming functional skeletal muscle cells? The answer, as it turns out, is that stem cells produce molecules that strongly promote muscle regeneration and muscle function.
Stem cells release these molecules in tiny packets called exosomes. Exosomes are tiny spheres that “bubble out” of stem cells, in a manner of speaking. Exosomes have a cell membrane, like cells themselves, but are much smaller, and they do not have the ability to reproduce. Instead, exosomes are highly packed with proteins, DNA, messenger RNA, micro RNA, cytokines, and other factors.
Nakamura and co-researchers showed exosomes can help regenerate muscle. These researchers showed that by injecting exosomes harvested from stem cells (without any of the stem cells themselves), they could increase muscle growth and blood vessel growth. In short, these molecules accelerate the rate at which muscles regenerate.
While more research is needed, this work suggests that exosomes retrieved from mesenchymal stem cells could be used to help regrow functional muscle in patients with various forms of muscle injury.
Reference: Nakamura et al. (2015). Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. FEBS Letters. 2015 May 8;589(11):1257-65.

by admin | Jan 4, 2019 | Stem Cell Research, Stem Cell Therapy, Studies
Spinal cord injury can be one of the most devastating
injuries. Long neurons that extend from the brain down the spinal cord are
severed and scarred. In most cases, this damage can never be repaired. If
patients survive an injury to the spinal cord, they can be permanently
paralyzed. Researchers have attempted to use high-dose steroids and surgery to
preserve the spinal cord, but these approaches are either controversial or
largely ineffective.
Ideally, one would create an environment in which nerve
cells in the spinal cord could regrow and take up their old tasks of sensation
and movement. One of the most promising approaches to do just this is stem cell
transplantation.
To test this concept, researchers used
stem cells derived from human placenta-derived mesenchymal
stem cell tissue (not embryonic stem cells) to form neural stem cells in
the laboratory. These neural stem cells have the ability to become neuron-like
cells, similar to those found in the spinal cord. The researchers then used
these stem cells to treat rats that had experimental spinal cord injury. The
results were impressive.
Rats treated with neural stem cells regained the partial
ability to use their hindlimbs within one week after treatment. By three weeks
after treatment, injured rats had regained substantial use of their hindlimbs.
The researchers confirmed that this improvement was due to neuron growth by
using various specialized tests (e.g. electrophysiology, histopathology). Rats
that did not receive stem cells did not regain substantial use of their
hindlimbs at any point in the study.
This work is particularly exciting because it shows that
stem cells can restore movement to animals who were paralyzed after spinal cord
injury. Moreover, the researchers used human stem cells derived from placenta,
which suggests that this effect could be useful in human spinal cord injury
patients (perhaps even more so than in rats). While additional work is needed,
these results offer hope to those who may one day develop severe spinal cord
injury.
Reference:
Zhi et al. (2014). Transplantation of placenta-derived
mesenchymal stem cell-induced neural stem cells to treat spinal cord injury.
Neural Regen Research, 9(24): 2197–2204.

by admin | Dec 14, 2018 | Parkinson's Disease, Stem Cell Research, Studies
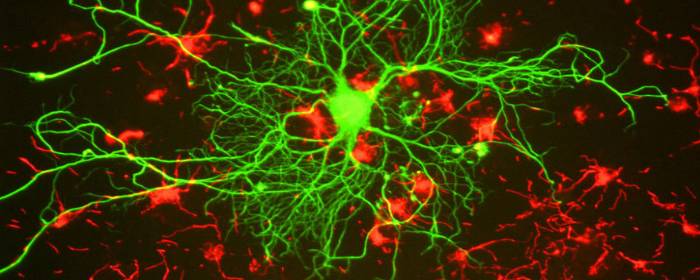
Parkinson’s disease is a progressive neurodegenerative disorder that causes tremor,rigidity, changes in facial expression, and several other symptoms. Whilesufferers usually retain their full cognitive abilities and memory, they tendto be impacted in mood and some mental health conditions that emerge as part ofthe condition process.
Parkinson’s disease is caused by loss of brain cells in a specific region of the brain called the substantia nigra. The neurons in this area of the brain contain dopamine, and as those nerve cells die, the levels of dopamine in the brain decrease. Consequently, patients with Parkinson’s disease often take medications that improve or accentuate dopamine signaling in the brain. These drugs can be effective for a certain period of time, but eventually, the condition will overcome the ability of these drugs to improve dopamine signaling. There is no cure for Parkinson’s disease, but researchers hope stem cells may be the answer.
Since dopamine drugs have worked reasonably well to control the symptoms of Parkinson’s disease, researchers assumed that replacing dopamine cells in the brain would help treat Parkinson’s disease. In a way, it did. When people with Parkinson’s disease received transplants of stem cells intended to produce dopamine, some of them experienced dramatic improvements in motor function. However, patients still had several other symptoms of Parkinson’s disease such as fatigue, bowel problems, sexual problems, and mood disorders. Neuroscience researchers realized Parkinson’s is not just about a loss of dopamine. It turns out, that while stem cells can help restore dopamine in people with Parkinson’s disease, they also coulduse help with serotoninneuron regenerating.
As a result of this groundbreaking work, researchers are now planning and implementing experiments in which Parkinson’s disease patients will receive stem cell transplants containing both dopamine cells and seroton in cells. If effective, we will be one step closer to a new and powerful treatment for Parkinson’s disease.
Reference: https://blogs.scientificamerican.com/scicurious-brain/parkinsons-is-much-more-than-dopamine/?WT.mc_id=send-to-friend

by admin | Dec 7, 2018 | Studies, Mesenchymal Stem Cells, Umbilical Stem Cell
Liver failure is a serious, potentially fatal condition in which large swaths of liver cells become dysfunctional and die. Liver failure is the result of several conditions including chronic alcohol consumption, exposure to drugs that are toxic to the liver (e.g. acetaminophen), autoimmune diseases, or infections such as hepatitis C. Liver failure causes several metabolic abnormalities including dangerously low levels of sodium, potassium, and phosphate in the blood. Moreover, four in 10 people with liver failure have trouble regulating their blood glucose levels, which can cause profound hypoglycemia. Since the liver detoxifies the blood, when the liver fails, patients can experience confusion from excessive amounts of ammonia and other substances in the blood. Seizures are also possible.
Short of liver transplantation, there are very few treatments for liver failure. Most treatments focus on restoring sodium, potassium, phosphate, and glucose levels in the blood, and bringing down ammonia levels. Fortunately, experiments show that human mesenchymal stem cells may be a promising treatment for liver failure.
Researchers enrolled 43 people with acute-on-chronic liver failure caused by hepatitis B infection. In this group, 24 patients were treated with mesenchymal stem cells derived from human umbilical cord and 19 patients received a saline solution. The groups received stem cells or placebo, respectively, three times every four weeks. Patients treated with mesenchymal stem cells showed better measures of liver function than those who received placebo. Livers of the patients treated with stem cells produced much more protein, albumin, and clotting factors, and were better able to process bilirubin. Importantly, no significant side effects were observed during the trial.
Given the serious nature of liver failure and the lack of effective treatments (besides liver transplant), this research is incredibly exciting. It offers hope that through further research scientists will be able to use mesenchymal stem cells to change the outcomes of people with acute-on-chronic liver failure.
Reference: https://stemcellsjournals.onlinelibrary.wiley.com/doi/abs/10.5966/sctm.2012-0034

by admin | Dec 3, 2018 | Osteoarthritis, Stem Cell Research, Studies
The human skeleton is made up of bone, cartilage, fat, nerves, blood vessels, and bone marrow. While the skeleton is usually strong and vibrant in youth, it changes considerably with age. Many people, especially women, experience demineralization of bone called osteoporosis. Most of us will suffer from painful, stiff, arthritic joints either from osteoarthritis or rheumatoid arthritis or both. While some of the diseases of bone and joints have specific treatments, none of them helps to restore bone and joints to their younger state. If one could reintroduce skeletal stem cells into the body, that could all change. Excitingly, researchers have recently isolated human skeletal stem cells from bone and other tissues.
At first glance, this breakthrough may not seem so surprising. One might wonder: didn’t we already have stem cells that form bone and cartilage? The answer is yes, but with an important caveat. Before researchers recently isolated human skeletal stem cells, the only stem cells that could be used to produce bone and cartilage were rather unpredictable. In addition to bone and cartilage, the mesenchymal stem cells that have been long used to form these tissues could also produce fat, muscle, fiberglass, blood vessel cells, and other tissues. In other words, the stem cells were broadly multipotent and, by extension, could not easily be used for a specific purpose, like mending bone or repairing an arthritic joint. That is why the recent discovery of these particular skeletal stem cells is so important.
The researchers isolated skeletal stem cells from various human tissues, mainly bone. They then used the skeletal stem cells to regrow bone and/or cartilage. Not only did the stem cells produce bone and cartilage in the first animal they tested, but they could retrieve stem cells from that animal and then cause bone to regrow in a second animal. This means that the skeletal stem cells have the capability of reproducing themselves.
The same researchers also discovered that when a skeleton is injured, such as in a bone fracture, the number of skeletal stem cells in that area increases dramatically. This makes sense since these cells are used to repair and regrow bone. It is also a promising result because it suggests that stem cells could be used to accelerate bone and joint healing in humans.
Scientists not directly involved in this research heralded this finding as “an extremely important advance.” However, they also acknowledge that more work needs to be done before skeletal stem cells can be routinely used in patients with orthopedic conditions. Nevertheless, these results are an exciting development in the field of stem cell research and orthopedics.
Reference: https://www.sciencenews.org/article/humans-have-skeletal-stem-cells-help-bones-and-cartilage-grow


 St. Petersburg, Florida
St. Petersburg, Florida
