
by admin | Jun 26, 2020 | Traumatic Brain Injury, Exosomes, Stem Cell Therapy
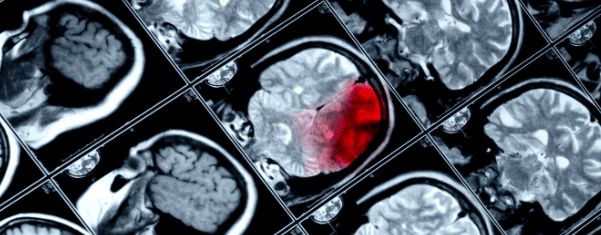
Traumatic brain injury is a single name given to a broad variety of conditions. In every instance of traumatic brain injury, some external force causes damage to the brain. This may be mild and short-lived, such as a concussion, or severe and permanent, such as severe head trauma. The initial trauma or injury can cause a number of injuries to the skull and brain such as skull fracture, cerebral contusion (“brain bruise”), cerebral edema (“brain swelling”), or hemorrhage (“brain bleed”).
Traumatic brain injury can also cause several secondary injuries that may continue for hours or days. The secondary effects of traumatic brain injury include:
- Electrolyte imbalances
- Mitochondrial dysfunction
- Inflammation
- Ischemia (lack of blood flow to parts of the brain)
- Brain cell destruction
These secondary traumatic brain injuries can cause long-term and even permanent neurological dysfunction.
Unfortunately, there are very few treatments for traumatic brain injury. Neurosurgeons can sometimes stop brain bleeding, stabilize skull fractures, and reduce brain swelling; however, there is little that can be done to stop the secondary effects of traumatic brain injury. Doctors have tried using steroids or hypothermia (cooling the patient) to decrease inflammation and stop further injury, but these interventions are not highly effective.
Ideally, one would give a treatment soon after a person has had a traumatic brain injury. This treatment would reduce or block the secondary effects of traumatic brain injury. Scientists are studying whether stem cell treatment can do that very thing.
Researchers recently showed that exosomes from bone marrow mesenchymal stem cells were able to reduce the secondary effects of traumatic brain injury. They humanely caused a traumatic brain injury in a group of mice. Fifteen minutes after the TBI, half the mice were given an injection of stem cells and the other half received a placebo (i.e. saltwater).
The mice that received the stem cell exosome treatment did substantially better than the mice who received a placebo. Stem cell exosome treatment substantially reduced the size of the damage to the brain compared to control. Moreover, mice that received stem cell exosome treatment did better on sensory, motor, reflex, and balance tests. In other words, stem cell exosome treatment helped mice with traumatic brain injury move better than those that did not receive stem cell exosome treatment.
The scientists went on to show that exosome treatment helped block the secondary effects of traumatic brain injury on the cellular and molecular level. In short, stem cell exosome treatment reduced inflammation in the brain from TBI.
Taken together, these results strongly suggest that treatment with exosomes from bone marrow mesenchymal stem cells soon after traumatic brain injury has the ability to protect the brain from damage. Of course, this treatment will need to be tested in humans who have had incidental TBI. Nevertheless, the basic science results are quite exciting since few neuroprotective agents, if any, can block the secondary effects of traumatic brain injury the way exosomes did in this scientific report.
Reference: Haoqi, N., et al. (2019). Exosomes Derived From Bone Mesenchymal Stem Cells Ameliorate Early Inflammatory Responses Following Traumatic Brain Injury. Frontiers in Neuroscience. 2019 Jan 24; 13:14.

by Stemedix | Jun 22, 2020 | Stem Cell Therapy, Multiple Sclerosis
Multiple sclerosis (MS) poses distinct challenges for many individuals. Not only does it present an array of frustrating symptoms ranging from muscle weakness and numbness to vision and bladder problems, but in some patients, it may resist medications altogether. For patients in search for an alternative option for relapse-remitting MS, researchers at Duke University School of Medicine are exploring a new potential therapy in a clinical trial: stem cell transplantation.
The trial, which is highly selective and randomized, will test the efficacy of stem cell transplantation of bone marrow against several different immune reconstitution therapies. Participants will include patients for whom disease-modifying therapies have been ineffective in the past.
While the study’s investigators acknowledge the risks that come with immunosuppression, they are also optimistic in the treatment’s ability to manage some of the most progressive forms of MS, calling stem cell transplantation “one of the most promising therapies” for the condition. By reconstituting the immune system through suppression and then introducing stem cells, the objective is to combat the inflammatory flares that occur in the brain and spinal cord every 12 to 15 months in this form of MS.
Immune reconstitution has already shown promise in the past, and people with MS who have undergone the treatment have witnessed the absence of new symptoms several years after pursuing the therapy. Compared to existing therapies, many of which have been around since the early 1990s, the treatment could hold enormous potential under the right circumstances. The trial’s team is working diligently to mitigate potential risks and thoroughly examine any individual risk factors with prospective participants. Contact a Care Coordinator today for a free assessment!

by admin | Jun 12, 2020 | Exosomes, Stem Cell Therapy
Many clinical studies have shown the safety and benefit of exosomes. As a result, numerous companies have been bringing exosome products to market. However, not all exosomes are the same. The cell type from which the exosomes are collected makes an enormous difference in safety and results.
Scientists have recently drawn attention to the fact that cell type matters when it comes to exosomes. Virtually every cell in the human body releases small packets of substances called exosomes. The number of exosomes and the substances inside exosomes can vary considerably, depending on the type of cell. Exosomes derived from stem cells and stromal cells have received the most research attention. That is because exosomes from stem cells contain most of the substances that provide a benefit to patients from stem cells. In other words, if you receive treatment of exosomes from stem cells, you are basically getting additional benefits from the exosomes that you would have gotten from just the stem cells themselves. However, the source of the stem cell exosomes matter.
Most of the research done in this area revolves around two types of stem cells: Exosomes taken from bone marrow mesenchymal stem cells and exosomes taken from placental mesenchymal stem cells. Bone marrow stem cells seem to have two major advantages over the placenta-derived stem cells. The first is that bone marrow stem cells have a stronger ability to modulate the immune system. The second is that bone marrow stem cells have immune privilege, which means they can avoid the body’s immune system. Specifically, placenta stem cell exosomes contain higher levels of PDL1 and HLA-G, which can make them more likely to provoke a negative immune response.
Surprisingly but reasonably, there have been of 63,000 scientific articles published on the safety and efficacy of bone marrow stem cells, but only about 1,200 on placenta stem cells.
Talk to your stem cell and exosome provider about your choices of exosomes, and make sure to ask from what cell type the exosomes are derived.
Reference: Hicok, Kevin & Vangsness, Thomas & Dordevic, Maxwell. (2020). Exosome Origins: Why the Cell Source Matters. 4. 1-4.

by Stemedix | Jun 8, 2020 | Autoimmune, Stem Cell Therapy
The immune system is divided into two major entities, depending on the type of action it exerts; the innate immune system and the specific immune system.
The innate immune system, which you can think of as the first responder to foreign pathogens that try to penetrate the body. This system is also referred to as non-specific immunity because it does not differentiate between different aggressors. The main components of the innate immune system include mechanical barriers (e.g., skin, acidic environment of the stomach, cilia found in the respiratory tract) and immune cells (e.g., macrophages, natural killers, neutrophils, basophils).
The specific immune system, which implements unique immune cells and antibodies to specifically target germs. For instance, when you get infected with the stomach flu, the immune system will produce specific cells and antibodies to the proteins found on the surface of that virus. As a result, it will be ready for the next aggressive episode since it has the necessary information to target the virus.
These two entities work to complement one another to keep us alive, with thousands of foreign pathogens destroyed every day. Now that you’re familiar with the immune system, let’s see how stem cell therapy may help in these cases.
What is an autoimmune disease?
An autoimmune disease is an inflammatory and immune reaction to self-antigens. In other words, the body will attack proteins found on harmless substances, such as blood cells, neurons, and pancreatic cells. Some examples of autoimmune diseases include lupus, multiple sclerosis, and rheumatoid arthritis.
Autoimmune diseases are poorly understood, hence the absence of any curative treatment. Most therapeutic approaches focus on long-term medical management that includes taking chemotherapeutic drugs, corticosteroids, and immunomodulators. Moreover, some severe cases may require surgical interventions.
Fortunately, recent research is showing positive results in patients who underwent stem cell therapy for their autoimmune disease using mesenchymal stem cells.
How does stem cell therapy help with autoimmune disease?
Stem cells have been extensively researched for their beneficial effects on several maladies, including the ones that get triggered by a defective immune system. The way that stem cells give this result is by repairing the damaged tissues and regulating the action of immune cells. Consequently, the cells will be less likely to attack self-antigens anymore, tempering down the symptoms of the condition.
Mesenchymal stem cells are a preferred type of cell that avoid ethical issues with extracting these cells and the efficacy they showed over the past few years. Researchers reported that MSCs focus most of their action on T regulatory cells that control the reaction of the specific immune system to foreign pathogens. If this line of cells is not well-regulated, the immune system will overreact to most antigens, resulting in the classic self-inflicted damage.
There are no cures for Autoimmune conditions, and some do find relief from traditional methods. However, there are risks and side effects to consider. Hopefully, a natural alternative option like stem cell therapy can provide additional options for those seeking treatment for autoimmune conditions. Contact us today for a free consultation!

by Stemedix | Jun 1, 2020 | Stem Cell Therapy, PRP
Orthopedic injuries occur each day and from different causes. An injury can result from a fall or a trauma to a musculoskeletal part of the body (e.g., knees, hips, shoulders). Many times, age or overuse can create a more common occurrence for these types of injury.
Some injuries are minor and the recovery is as easy as rest and at-home recovery methods. Other more serious injuries may require surgery and physical therapy to return to normal function. Some patients, however, may never recover fully and develop complications related to the initial trauma, such as decreased range of motion, chronic pain, psychological issues, or risks from surgery.
Today, regenerative medicine has presented innovative biological advances that offer an opportunity to address their medical issues in innovative ways that involve using biomedical therapies, such as platelet-rich plasma therapy and stem cell therapy.
What Is Platelet-Rich Plasma (PRP) Therapy?
Platelet-rich plasma (PRP) is a substance featuring concentrated platelets and proteins which are derived from whole blood. When the platelets are isolated and their concentration is increased, their growth factors are amplified by five to ten times.
This concentrated solution holds tremendous potential for promoting wound-healing and accelerating the process of regenerating lost tissue to help patients regain their physical function as soon as possible and relieve their pain.
Platelet-rich plasma (PRP) treatment is widely regarded as a safe and effective therapy since it is one’s own blood source. The potential benefits can be decreased pain, medication intake reduction, promotion of faster healing rate, slowing down of cartilage destruction, and stimulates cell growth and repair at site of injury.
In a 2014 study, scientists analyzed the effects of PRP therapy when associated with ultrasound guidance. They concluded that “According to the current results, which document full muscle recovery and no relapse except for one case, platelet-rich plasma ultrasound-guided injection represents a valid mini-invasive treatment for muscle injuries.”
What Is Stem Cell Therapy?
Stem cells are undifferentiated cells that can develop into various cell types and tissues. Scientists were extremely enthusiastic about the therapeutic potential of these cells in restoring damaged tissues, the functionality of organs, and managing symptoms brought on by chronic and degenerative conditions such as Rheumatoid Arthritis, Traumatic Brain Injury, and Multiple Sclerosis.
Many studies have used various types of stem cells in the treatment of different types of sports injuries. Mesenchymal Stem Cell (MSCs) is one of the most common stem cells in today’s research and applications. They are sourced from various tissues; adipose (fat) tissue, bone marrow, and the umbilical cord tissue.
In a 2017 review, scientists reveal the beneficial outcomes of mesenchymal stem cells from eight different studies. The studies were performed on patients that had varying degrees of osteoarthritis. The findings concluded were promotion of cartilage regeneration, reduction of pain, and improved joint function. In addition, they were able to determine that the more stem cells used, the better the outcome of the therapy.
What Is The Difference Between These Two Treatments?
Despite the similar regenerative properties that both treatment options offer, there is a clear difference in their mechanisms of action, as PRP therapy focuses on the recruitment of immune cells, growth factors, and hormones to stimulate the regeneration of the damaged tissue.
On the other hand, stem cell therapy works by replacing the basic building blocks of the damaged tissue, which are the cells. Simply put, stem cells will differentiate into myocytes chondrocytes, osteocytes, fibroblasts, and other cells found in the muscle/joint capsule to restore the physical function of patients.
Regardless of these differences, they are both promising options due to their non-invasiveness, quick results, and lack of any serious side effects. Contact us today for a free consultation!

by Stemedix | May 25, 2020 | Stem Cell Therapy, Traumatic Brain Injury
Traumatic brain injury (TBI), also known as concussion, is a common condition that affects thousands of people every year in the United States alone. The most challenging aspect of TBI is its vague clinical presentation, which makes it difficult for physicians to promptly diagnose and treat this condition without a proper history of trauma.
According to the Centers for Disease Control and Prevention (CDC), the number of TBI-related hospital visits and deaths increased by 53% between 2006 and 2014. Unfortunately, patients who survive after a concussion often deal with neurological sequela for the rest of their lives. This article will explore the basic concepts of TBI as well as the role of stem cell therapy in restoring normal neurological function after irreversible damage.
How Do Concussions Happen?
The brain is a fragile organ that’s protected by a boney structure known as the skull. Unfortunately, this protection can be a double-edged sword. To prevent contact between the brain and the skull, a liquid called cerebrospinal fluid (CSF) acts as a shock absorber to avoid any trauma to the brain when the skull is abruptly moved. In other words, the brain is floating in the CSF to be able to easily move around when you change positions.
A concussion occurs when the brain collides with the skull at an intensity that surpasses the CSF-cushioning ability. Consequently, the brain will shrink on itself, sending shock waves through the entire tissue, which tear the neurons. This phenomenon is referred to as diffuse axonal injury. As a result, the interneural network responsible for every task that the brain completes is compromised and may lead to irreversible loss of function.
Stem Cell Therapy and Traumatic Brain Injury
Stem cells have the ability to differentiate into several body tissues, which makes them a candidate to treat and repair damage for a myriad of medical conditions, including traumatic brain injuries.
In a clinical trial, researchers used bone marrow-derived stem cells as repair agents to restore the function of damaged brain tissue after enduring TBI. Stem cells were introduced to patients using minimally-invasive procedures with highly-sensitive imaging guidance to deliver the cells at the exact site of tissue damage.
Researchers stated that “These stem cells secrete growth factors that have shown preclinical benefit and also recruit the patient’s own stem cells through various homing signals. Recent successes with similar stem cell therapy trials in other diseases, such as for heart attack recovery, have generated increased interest in now using these approaches to treat brain injury.”
Moreover, a 2018 study published by nature, scientists aimed to find out if certain types of cell therapy, such as umbilical cord stem cells and bone marrow-derived stem cells benefit patients with traumatic brain injuries. The researchers found that these cells can regenerate neurons and repair damage, which may revolutionize the field of traumatology since patients may restore certain neurological functions even after irreversible damage.
Note that the idea of using stem cell therapy to treat concussions is not new, as a 2002 experimental study on rats concluded that “We show for the first time that the IV administration of human umbilical cord blood cells reduces functional deficits after severe traumatic brain injury in the rat. The injected cells enter the brain, migrate into the injured area, and a few express the neuronal and astrocytic phenotypes and integrate into the vascular structures. Cord blood administration may be a useful treatment for traumatic brain injury.”
The use of stem cell therapy to manage symptoms of TBI are still in the experimental phases; however studies have shown its potential to restore lost functions with minimally-invasive procedures that carry an extremely safe side effect profile.
Contact us today!


 St. Petersburg, Florida
St. Petersburg, Florida
