
by admin | Jul 8, 2019 | Exosomes, Osteoarthritis, Stem Cell Research, Stem Cell Therapy
Osteoarthritis is the most common form of arthritis. About one in 10 people will develop osteoarthritis at some point in their lifetimes. As the condition progresses, synovial membranes and cartilage break down. Osteoarthritis causes people to experience joint pain, joint stiffness, and restricted movement. Knees, hips, and hands are common sites for arthritis, though people can experience the condition in virtually every joint in the body including joints and spine. Mild osteoarthritis may be nothing more than an annoyance, but moderate and severe osteoarthritis can diminish a person’s quality of life and cause substantial suffering and disability.
Despite the commonness of osteoarthritis, there are very few effective treatment options. People may take pain medications to help cope with discomfort; however, taking these medications every day can lead to unwanted side effects. Physical therapy, braces, walking aids, and exercise may have some effect, but their benefit is unpredictable, i.e., these approaches work for some people and not others. The only definitive treatment for osteoarthritis is to replace the joint with an artificial one; however, orthopedic surgery is expensive, associated with a long recovery, and is usually only an option after patients have suffered pain and disability for a long period of time.
Ideally, osteoarthritis treatment would be focused on restoring the structure of the damaged joint itself. For a time, physicians were hopeful that glucosamine and chondroitin could do this. These two substances are diminished in osteoarthritis, so the concept was to replace them and hopefully rebuild damaged joints. While initial clinical studies seemed to suggest glucosamine and chondroitin were helpful, larger, high-quality clinical trials failed to show any benefit. Nevertheless, the goal of repairing joints damaged by osteoarthritis is still a top goal. Now, however, scientists have turned to stem cells instead of small molecules.
Stem cell researchers are particularly interested in the small sacs released by stem cells called exosomes. Exosomes contain proteins, RNA, cytokines, and other substances that are important for tissue regeneration. Exosomes are apparently responsible for most of the clinical benefit of stem cells in the first place. Moreover, it is much more convenient for doctors to use exosomes as treatment rather than stem cells themselves.
To this end, researchers have been studying the effects of stem cell exosomes. One research group recently published a report studying the effects of exosomes that were collected from synovial membrane stem cells and compared them to exosomes taken from induced pluripotent stem cells. Synovial membrane stem cells are an obvious choice for treating osteoarthritis since synovial membranes are one of the substances that break down in the disease. However, synovial membrane stem cells are difficult to obtain. It is far more practical to use induced pluripotent stem cells since there is a virtually limitless supply of them.
The researchers compared exosomes taken from these two types of stem cells in mice with experimental osteoarthritis. Not only did the scientists show that exosomes taken from pluripotent stem cells were highly effective in treating osteoarthritis, these exosomes were even more effective in treating osteoarthritis then exosomes taken from synovial membrane stem cells. Exosomes from pluripotent stem cells not only repaired synovial membranes but they also helped replace cartilage by stimulating chondrocytes (cartilage cells).
Of course, this work will need to be confirmed in humans with osteoarthritis; however, the results of this animal research are very encouraging. In short, this research suggests that exosomes taken from induced pluripotent mesenchymal stem cells may be a convenient and effective way to treat osteoarthritis in the future.
Reference: Zhu, Y. et al. (2017). Comparison of exosomes secreted by induced pluripotent stem cell-derived mesenchymal stem cells and synovial membrane-derived mesenchymal stem cells for the treatment of osteoarthritis. Stem Cell Research and Therapy. 2017 8:64.

by admin | Jun 25, 2019 | Stem Cell Research
Men with erectile dysfunction cannot achieve or maintain an erection suitable for sexual intercourse. Erectile dysfunction can be devastating for the men who suffer from it, putting a strain on intimate relationships, and causing significant emotional suffering. Sadly, half of all men between the age of 40 and 70 experience some degree of erectile dysfunction. Fifteen percent of men are completely impotent, and many men do not respond to typical treatments.
Many men with erectile dysfunction can be successfully treated with phosphodiesterase type-5 inhibitors such as Viagra or Cialis. These pills can be taken daily or as needed to allow men to achieve erections when desired. However, these medications have some significant side effects. For example, these drugs can cause an unsafe drop in blood pressure, especially in people who are taking nitrate medications for heart and cardiovascular diseases. Likewise, these drugs can be expensive, since they are not always covered by insurance programs.
It also should be pointed out, that not all men find success from these erectile dysfunction drugs and must turn to penile injections. Penile injections are particularly inconvenient because an injection must be performed prior to each sexual encounter.
Since most men who suffer from erectile dysfunction have problems with the blood vessel system that makes erections possible, scientists have been investigating the possibility of using stem cells to help regenerate and regrow the cells in that system. While there have only been a handful of clinical trials using stem cells to treat erectile dysfunction, the results are promising.
Bahk and co-authors used umbilical cord stem cells to treat seven men with erectile dysfunction related to their type 2 diabetes. Almost all of the men who received a penile injection of stem cells experienced a return of morning erections and reported an increase in penile hardness. This effect lasted for at least three months after the injection.
Another research group tested adipose (fat tissue) stem cells in men who had erectile dysfunction due to prostate removal surgery. Some of these men also lost their ability to control urine (i.e. urinary incontinence). Eight of 17 men in the trial recovered erectile function. Interestingly, the incontinent men were the ones I the group of 17 who failed to achieve a benefit from stem cell injections.
Lastly, researchers tested stem cells taken from placental tissues (not embryonic stem cells) in men with erectile dysfunction of unknown cause. Men who were treated with stem cells enjoyed a significant increase in blood flow and blood pressure to the penile area. Likewise, several men regained the ability to achieve and sustain erections even though they had been completely impotent before the treatment.
While this research is ongoing, these results are incredibly encouraging for men (and their partners) who struggle with erectile dysfunction. The benefits of stem cells are particularly relevant for men who do not receive any or complete improvement in erectile dysfunction from ED medications. While these treatments do require a penile injection, the effects tend to last much longer than current, non-stem cell penile injections (three months or longer), which is an important innovation and makes treatment far more convenient for patients.

by admin | Jun 19, 2019 | ALS, Stem Cell Research
Amyotrophic Lateral Sclerosis (ALS) causes muscle weakness that gets worse over time. This muscle weakness can be so disabling that patients may require devices to support movement and breathing. There are few drug treatments for ALS, if any, that make a meaningful difference in patients’ lives. Drugs such as riluzole and edavarone may slow the disease or help make the symptoms of ALS less troublesome; however, these drugs are only useful for a short period of time, if at all. People with amyotrophic lateral sclerosis ultimately die from this horrendous disease.
While the cause of ALS isn’t fully understood, nerves in the brain and spinal cord do become sick and eventually die. Without healthy nerve cells to control their muscles, patients with ALS experience increasing weakness, pain, and spasms.
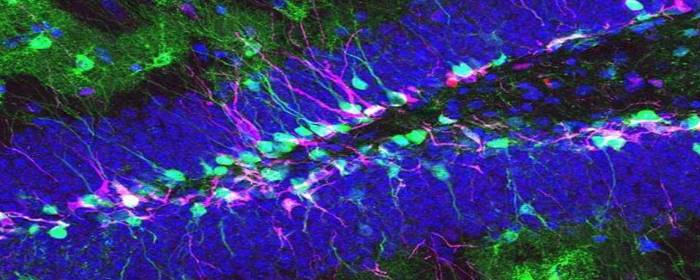
A group of researchers conducted two clinical trials to test human stem cells in patients with amyotrophic lateral sclerosis. The researchers chose a particular type of stem cell, taken from the spinal cord, called neural stem cells. A neural stem cell can become a neuron, an astrocyte, or an oligodendrocyte—all of which are important for the function of the brain and spinal cord. The goal of this research was to see if these neural stem cells could stop or delay the progression of ALS. In other words, could these human stem cells slow down how fast ALS gets worse, even for a short time?
As expected, the researchers found that ALS patients treated with human neural stem cells continued to get worse. However, the rate at which they got worse appeared to slow down slightly. The researchers clearly showed the treatment did not make the disease worse, and the treatment was generally safe and well tolerated. The researchers note that because of the small number of patients, they were unable to make strong conclusions about the therapy. On the other hand, the researchers were able to use these clinical trial results to design larger clinical trials to be held in the future. And, since this stem cell treatment is apparently safe, they should be able to expand to larger numbers of ALS patients.
Reference: Glass, JD. et al. (2016). Transplantation of spinal cord-derived neural stem cells for ALS: Analysis of phase 1 and 2 trials. Neurology. 2016 Jul 26;87(4):392-400.

by admin | May 30, 2019 | Lupus, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Umbilical Stem Cell
Systemic lupus erythematosus or simply “lupus” is a chronic inflammatory disease that can affect almost every organ and tissue in the body. Most people are aware of chronic fatigue, muscle and joint pain, and a characteristic facial skin rash that occurs in people with lupus. However, the disease can affect the gastrointestinal tract, lungs, heart, eyes, lymph nodes, and brain. About half of all people with lupus will develop problems in their kidneys related to the disease. The most common kidney problem caused by lupus is a condition known as lupus nephritis.
Lupus nephritis may not cause any outward symptoms, though some patients report foamy urine. Physicians usually detect lupus nephritis during routine urinalysis. Lupus nephritis causes the kidneys to leak substantial amounts of protein in the urine. Over time, this protein loss can cause swelling in the hands, ankles, and feet, and may interfere with kidney function.
The main way in which lupus nephritis is treated is by using strong immunosuppressants such as glucocorticoids (“steroids”; prednisone), cyclophosphamide or mycophenolate mofetil. These immunosuppressing drugs can cause a number of serious and perhaps permanent side effects. Making matters worse, some people with lupus continue to have worsening lupus nephritis even after using these immunosuppressive drugs. In these cases, there is very little that can be done to treat the disease.
In order to help this group of individuals for whom regular treatments did not stop lupus nephritis from progressing, researchers conducted a clinical trial to test the effect of stem cells on this illness. Researchers collected allogeneic mesenchymal stem cells from bone marrow and umbilical cord tissue. They then infused the stem cells in 81 patients with lupus nephritis and followed them for 12 months. Amazingly, 60.5% of patients enjoyed remission of their kidney disease by the 12-month visit. Kidney function (glomerular filtration rate; GFR) significantly improved in patients treated with mesenchymal stem cells. Likewise, total lupus disease activity (not just lupus nephritis) improved significantly 12 months after treatment. These improvements were so profound that patients were able to reduce their doses of prednisone and other immune-suppressing drugs. Importantly, the stem cells did not cause any apparent adverse effects.
If this work can be confirmed in subsequent clinical trials, it is exciting news for patients with lupus, especially those with lupus nephritis. This work suggests that stem cells may be able to reduce the doses of immunosuppressants currently used to treat lupus nephritis, and it may even stop the progression of this terrible illness in some patients. We eagerly await additional clinical research in this area.
Reference: Gu F et al. (2014). Allogeneic mesenchymal stem cell transplantation for lupus nephritis patients refractory to conventional therapy. Clinical Rheumatology. 2014 Nov;33(11):1611-9.

by admin | May 22, 2019 | Bone Marrow, Mesenchymal Stem Cells, Stem Cell Research, Stem Cell Therapy, Umbilical Stem Cell
Mesenchymal stem cells have two unique and powerful properties that make them the focus of intense scientific research. First, mesenchymal stem cells can escape recognition by the immune system. In other words, when mesenchymal stem cells are infused into the body, the immune system does not recognize them as foreign and does not react to them. If the immune system did respond to the stem cells, it would cause an aggressive and potentially deadly allergic or immunologic response. Second, mesenchymal stem cells have the power to inhibit the immune system. This means mesenchymal stem cells could be used to treat immunological and autoimmune diseases such as Rheumatoid Arthritis, Systemic Lupus Erythematosus, Multiple Sclerosis, and Crohn’s Disease, among others. In essence, mesenchymal stem cells can affect the immune system without triggering an inflammatory response making them an ideal treatment for these diseases.
For some time, mesenchymal stem cells extracted from bone marrow were thought to be the only type of mesenchymal stem cells capable of beneficially affecting the immune system. This fact is not necessarily bad, but it does mean that mesenchymal stem cell donors must undergo a bone marrow procedure, which can be painful and expensive. It would be far better if doctors could use mesenchymal stem cells taken from easier-to-get tissues such as fat (adipose), umbilical cord blood, or Wharton’s jelly (umbilical cord tissue). Most people have adequate amounts of fat just under the skin, and umbilical cord blood and tissue are thrown away as medical waste every day.
Fortunately for patients, Dr. Yoo and colleagues showed that mesenchymal stem cells taken from fat tissue, umbilical cord blood, and Wharton’s jelly exhibit the same immunomodulatory properties as mesenchymal stem cells taken from bone marrow. The researchers showed that these types of mesenchymal stem cells were able to suppress T-cell proliferation as effectively as those cells taken from bone marrow. T-cell proliferation, it should be pointed out, is a key step in autoimmune inflammation that occurs in diseases such as rheumatoid arthritis and others.
In short, mesenchymal stem cells taken from easier-to-get tissues were just as effective at suppressing inflammation (in vitro) as those taken from bone marrow. These results will need to be confirmed in clinical studies; however, this approach will be much more convenient and less expensive for patients and donors if they can use mesenchymal stem cells taken from fat or umbilical cord rather than bone marrow and yet reap the same benefits.
Reference: Yoo KH et al. (2009). Comparison of immunomodulatory properties of mesenchymal stem cells derived from adult human tissues. Cell Immunology. 2009;259(2):150-6.

by admin | May 16, 2019 | Mesenchymal Stem Cells, Multiple Sclerosis, Stem Cell Research, Stem Cell Therapy
A new study has shown that a protocol for treating Multiple Sclerosis with stem cells is safe. According to the researchers, the potential for using stem cells in Multiple Sclerosis therapy warrants further investigation. The results of the study were published in the Journal of Translational Medicine.
Stem cells – and specifically, mesenchymal stem cells, have been increasingly used in the treatment of immune and inflammatory conditions. Based on the success that has been seen in these areas, scientists reasoned that mesenchymal stem cells may also represent a useful approach to treat Multiple Sclerosis, a neurological disease that involves the abnormal attack by the immune system on the myelin sheath that insulates nerves and allows nerve cells to communicate effectively and efficiently with one another.
To test this idea, the scientists used umbilical cord mesenchymal stem cells in 20 Multiple Sclerosis patients. The patients were given intravenous injections of the stem cells each day for seven days. The researchers evaluated the patients – with both neurological testing and nervous system imaging – at baseline, one month after treatment, and one year after treatment. The researchers found that the stem cell treatment improved neurological scores in patients and that lesions in the brain and cervical spinal cord were inactive one year after the stem cell injections. There were no serious adverse side effects associated with the treatment.
Based on these findings, it is possible that stem cells will provide a useful treatment option for those with Multiple Sclerosis. With more research, we will better understand exactly how stem cells can be used to help this population of patients.
Reference: Riordan, N.H. et al. (2018). Clinical feasibility of umbilical cord tissue-derived mesenchymal stem cells in the treatment of multiple sclerosis. Journal of Translational Medicine, 16(57), 1-12.





 St. Petersburg, Florida
St. Petersburg, Florida
