
by admin | Jan 14, 2019 | Stem Cell Research, Stem Cell Therapy, Stroke
Patients who suffer ischemic stroke have some treatment
options, but many of them require immediate intervention and so are not useful
if too much time has elapsed between the stroke and treatment. Therapies that
employ stem cells are promising alternatives because stem cells can differentiate
into brain cells and potentially help to replace tissue that has been damaged
or destroyed.
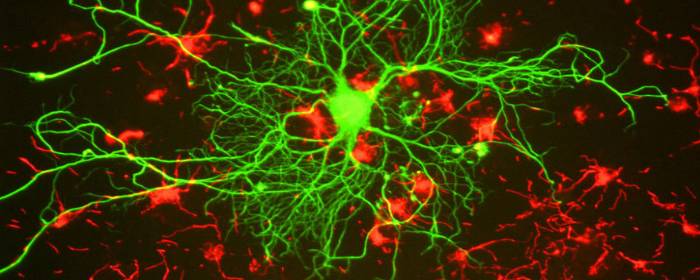
A recent study published in Stem Cells
and Development has shown for the first time that a specific type of stem
cell – called ischemia-induced multipotent stem cells – may be able to help
with such repair of brain tissue in patients who have suffered a stroke.
Specifically, the research team demonstrated the technical ability to isolate
the ischemia-induced multipotent stem cells from the brains of elderly stroke
patients.
The scientists then used protein
binding techniques to determine where in the brain these stem cells came from.
They found that the cells came from areas of the brain where brain cells had been
damaged or killed from the stroke. These cells were located near blood vessels
and expressed certain biological markers that enabled the researchers to
confirm that they qualified as stem cells. Specifically, these cells had
proliferative qualities that suggested that they could potentially be used to
re-populate damaged areas of the brain. The cells also showed the ability to
differentiate into different types of cells, a key characteristic of stem cells
used for therapeutic purposes.
This study represents a
significant step in overcoming the technical challenges associated with
isolating and classifying ischemia-induced multipotent stem cells. The next
step for researchers will be to test the potential of these cells in stroke
treatment. If researchers show that these stem cells can be used to
successfully repair damaged areas of the brain – and more importantly, restore
functions that were disrupted by the stroke – then physicians and scientists
may be able to work together to translate these findings into therapies that
are regularly used in stroke.
Reference
Tatebayashi et al. 2017. Identification of multipotent stem
cells in human brain tissue following stroke. Stem Cells and Development, 26(11), 787-797.

by admin | Jan 4, 2019 | Stem Cell Research, Stem Cell Therapy, Studies
Spinal cord injury can be one of the most devastating
injuries. Long neurons that extend from the brain down the spinal cord are
severed and scarred. In most cases, this damage can never be repaired. If
patients survive an injury to the spinal cord, they can be permanently
paralyzed. Researchers have attempted to use high-dose steroids and surgery to
preserve the spinal cord, but these approaches are either controversial or
largely ineffective.
Ideally, one would create an environment in which nerve
cells in the spinal cord could regrow and take up their old tasks of sensation
and movement. One of the most promising approaches to do just this is stem cell
transplantation.
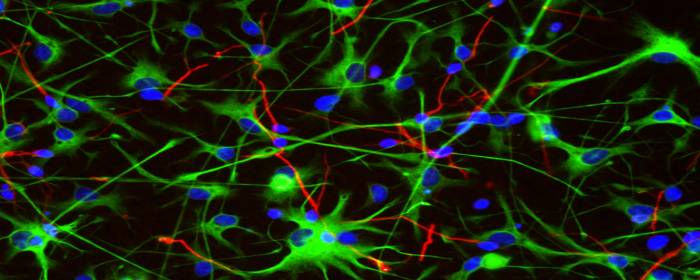
To test this concept, researchers used
stem cells derived from human placenta-derived mesenchymal
stem cell tissue (not embryonic stem cells) to form neural stem cells in
the laboratory. These neural stem cells have the ability to become neuron-like
cells, similar to those found in the spinal cord. The researchers then used
these stem cells to treat rats that had experimental spinal cord injury. The
results were impressive.
Rats treated with neural stem cells regained the partial
ability to use their hindlimbs within one week after treatment. By three weeks
after treatment, injured rats had regained substantial use of their hindlimbs.
The researchers confirmed that this improvement was due to neuron growth by
using various specialized tests (e.g. electrophysiology, histopathology). Rats
that did not receive stem cells did not regain substantial use of their
hindlimbs at any point in the study.
This work is particularly exciting because it shows that
stem cells can restore movement to animals who were paralyzed after spinal cord
injury. Moreover, the researchers used human stem cells derived from placenta,
which suggests that this effect could be useful in human spinal cord injury
patients (perhaps even more so than in rats). While additional work is needed,
these results offer hope to those who may one day develop severe spinal cord
injury.
Reference:
Zhi et al. (2014). Transplantation of placenta-derived
mesenchymal stem cell-induced neural stem cells to treat spinal cord injury.
Neural Regen Research, 9(24): 2197–2204.

by admin | Dec 29, 2018 | Mesenchymal Stem Cells, Osteoarthritis, Stem Cell Therapy
Most large joints of the body contain cartilage, a substance that is softer and more flexible than bone. Because of its softness and flexibility, cartilage is well-suited to protect the bones as they move across one another. Unfortunately, this softness and flexibility also makes cartilage prone to injury and erosion. In patients with osteoarthritis, forexample, cartilage breaks down to the point that bone rubs against bone,causing pain and disability. Certain injuries can damage the cartilage (i.e.osteochondral lesion), which can essentially have the same effect.
Once the cartilage of joints has become damaged, there is
little that can be done to fix it. Patients may receive steroid injections into
the joint to reduce inflammation, and may rely on pain medications to relieve
the pain and swelling. Short of joint replacement therapy, no treatments can
reverse cartilage damage once it has occurred.
Fortunately, mesenchymal stem cells may soon be able to reverse cartilage defects that arise from osteochondral lesions and osteoarthritis. Wakitani and colleagues took samples of patients’ bone marrow, which contains mesenchymal stem cells. They then used various laboratory techniques to increase the number of stem cells in the sample. Four weekslater, the researchers then reinjected the concentrated stem cells back intothe same patient using their own source of stem cells. The Wakitani groupshowed that stem cell transplantation improved the patient’s clinical symptoms bysix months, a benefit that continued for two years on average. Samples takenfrom the patients 12 months later showed that the damaged cartilage had beenrepaired. In other work, Centeno and co-authors showed that bone marrow-derived mesenchymal stemcells could increase the volume of cartilage, reduce pain, and increase rangeof motion 24 weeks after stem cell transplantation.
Research continues to determine which stem cells are most useful, how many stem cells should be injected, how many injections need to be administered, and how should those stem cells be prepared before they are injected? Nonetheless, certain groups are making great strides in this area. In fact, the recent discovery of human skeletal stem cells promises to accelerate stem cell research into treating disorders of bone and cartilage.
Reference
Schmitt et al. (2012). Application of Stem Cells in Orthopedics. Stem Cells International. 2012: 394962

by admin | Dec 27, 2018 | Stem Cell Research, Stem Cell Therapy
A number of different stem cell types have been shown to exert significant therapeutic effects when transplanted into the central nervous system. These cells include non-hematopoietic stem cells such as mesenchymal stem cells and neural/progenitor stem cells and carry out their effects by secreting what are known as neurotrophic paracrine factors, whichhelp to control the immune system.
In recent years, it has been suggested that rather than requiring the injection of stem cells, brain injury repair may be achieved by injecting the molecules that stem cells tend to secrete – known as secretome. The stem cell secretome includes growth factors as well as cytokines and chemokines. Investigators have begun to explore whether delivering these substances, rather than stem cells, could offer a more efficient means to therapy.
The rationale is that by delivering these substances directly, it should be possible to stimulate the proliferation of progenitor cells in the central nervous system and therefore instigate repair. However, initial studies have shown that the infusion of individual cytokines does not have the expected effect. According to the authors of a review published in Biochimie, it may be that multiple substances will need to be simultaneously infused in pre-tested concentrations so that they can act synergistically to optimize therapeutic effects.
Clinical trials are underway to determine the safety to patients of the secretome approach and to identify any relevant risks so that potential risks can be weighed against potential benefits of this type of therapeutic approach. There is also research on a wide variety of topics that will need clarification if effective stem cell secretome therapies are to be developed for brain repair. These topics include clarifying aspects of tissue transport and determining the mechanisms by which secretomes confer their benefits.
Reference: Drago, D. (2014). The stem cell secretome and its
role in brain repair. Biochimie, 95(12),
2271-2285.

by admin | Dec 14, 2018 | Parkinson's Disease, Stem Cell Research, Studies
Parkinson’s disease is a progressive neurodegenerative disorder that causes tremor,rigidity, changes in facial expression, and several other symptoms. Whilesufferers usually retain their full cognitive abilities and memory, they tendto be impacted in mood and some mental health conditions that emerge as part ofthe condition process.
Parkinson’s disease is caused by loss of brain cells in a specific region of the brain called the substantia nigra. The neurons in this area of the brain contain dopamine, and as those nerve cells die, the levels of dopamine in the brain decrease. Consequently, patients with Parkinson’s disease often take medications that improve or accentuate dopamine signaling in the brain. These drugs can be effective for a certain period of time, but eventually, the condition will overcome the ability of these drugs to improve dopamine signaling. There is no cure for Parkinson’s disease, but researchers hope stem cells may be the answer.
Since dopamine drugs have worked reasonably well to control the symptoms of Parkinson’s disease, researchers assumed that replacing dopamine cells in the brain would help treat Parkinson’s disease. In a way, it did. When people with Parkinson’s disease received transplants of stem cells intended to produce dopamine, some of them experienced dramatic improvements in motor function. However, patients still had several other symptoms of Parkinson’s disease such as fatigue, bowel problems, sexual problems, and mood disorders. Neuroscience researchers realized Parkinson’s is not just about a loss of dopamine. It turns out, that while stem cells can help restore dopamine in people with Parkinson’s disease, they also coulduse help with serotoninneuron regenerating.
As a result of this groundbreaking work, researchers are now planning and implementing experiments in which Parkinson’s disease patients will receive stem cell transplants containing both dopamine cells and seroton in cells. If effective, we will be one step closer to a new and powerful treatment for Parkinson’s disease.
Reference: https://blogs.scientificamerican.com/scicurious-brain/parkinsons-is-much-more-than-dopamine/?WT.mc_id=send-to-friend




 St. Petersburg, Florida
St. Petersburg, Florida
