
by admin | Feb 24, 2020 | Aesthetics, Exosomes
Atopic dermatitis, better known as eczema, is a chronic, itchy skin disease. People with eczema have chronically dry skin, often in patches, that can be intensely itchy. The patches of atopic dermatitis vary from red bumps (papules or vesicles) when they are inflamed, to dry, scaly, pink areas when they are not inflamed. Patients with eczema itch so frequently that the skin in the lesion can thicken and harden, a process called lichenification. Even patients who manage to clear the lesions usually have a recurrence (i.e. the itchy patches come back).
Patients with eczema can try lotion and moisturizers to
soften the skin and reduce itchiness, but these are only helpful temporality
and only seem to work for people with mild disease. Often, topical
corticosteroids are required. Steroids are applied to areas of atopic
dermatitis to reduce inflammation and itchiness. In severe cases where steroids
are not fully helpful, light therapy (phototherapy) may be needed. Patients may
require more intense therapy for atopic dermatitis such as cyclosporine, methotrexate,
azathioprine, mycophenolate mofetil, or dupilumab. These medications have their
own set of side effects, so they are reserved for people with severe, chronic
eczema. Certainly better, safer treatments for atopic dermatitis are needed.
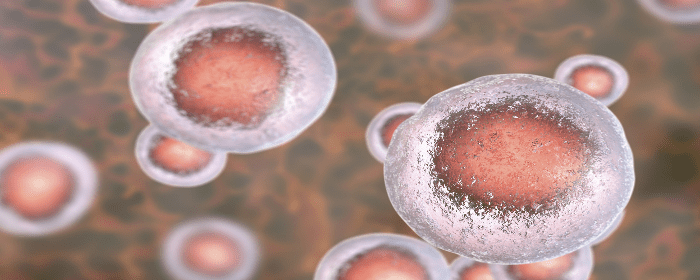
To this end, researchers conducted the first of its kind study to answer whether exosomes retrieved from mesenchymal stem cells taken from human adipose tissue (i.e. fat tissue) could relieve symptoms of atopic dermatitis in laboratory mice. Mice with experimental atopic dermatitis have similar symptoms to humans with the disease; they have itchy, red lesions that cause the skin to thicken. In the research study, treatment with stem cell-derived exosomes significantly improved the clinical score in these mice. In other words, stem cell exosome treatment reduced redness, swelling, scaling, dryness, and itching. Exosome treatment also reduced objective signs of inflammation including inflammatory cytokines (TNF, IL4, etc.), inflammatory antibodies (IgE), and inflammatory cells (eosinophils).
These results indicate that treatment with stem cell-derived
exosomes substantially reduced symptoms in mice with atopic dermatitis. Of
course, this work needs to be replicated in humans, but this important work
lays the foundation for future clinical trials.
Reference: Cho, BS. et al. (2018). Exosomes derived from
human adipose tissue-derived mesenchymal stem cells alleviate atopic
dermatitis. Stem Cell Research & Therapy. 2018, Jul 11;9(1):187.

by admin | Feb 17, 2020 | Kidney Disease
Stem cells have been used to repair and regenerate tissue and have been shown in recent years to have the plasticity necessary to improve conditions of solid organs. Given the success of bone marrow stem hematopoietic stem cells in this type of regenerative medicine, scientists have speculated that bone marrow stem cell mobilizers may be beneficial for treating organs that have undergone injury. Let’s discover stem cells for acute kidney injury and what potential they have for this condition.
Bone marrow stem cell mobilizers are substances that act to encourage stem cells from the bone marrow to move into the blood, where they can be collected, stored, and later used to replace bone marrow via a stem cell transplant. A recent paper published in Current Protein and Peptide Science covers about a decade of research on two bone marrow stem cell mobilizers, granulocyte colony-stimulating factor (G-CSF) and Plerixafor (AMD3100).
G-CSF is a
glycoprotein that stimulates both stem cells and granulocytes to be released by
bone marrow and enter the bloodstream. It is produced by a variety of tissues
and immune cells and functionally acts as both a cytokine and a hormone.
Plerixafor also stimulates the immune system and is used in patients with
multiple myeloma and non-Hodgkin lymphoma.
According to the authors, the preclinical studies on the impact of these stem cell mobilizers confirm that these mobilizers may be an effective way to therapeutically approach with stem cells for acute kidney injury. While more research is needed to determine exactly how these bone marrow stem cell mobilizers act in acute kidney injury and what role they may play in therapy, these initial data appear to justify more investigations into the value of these substances for kidney care.
Reference: Xu, Y. et al. (2017). Stem cell mobilizers: Novel
therapeutics for acute kidney injury. Current
Protein Peptide Science, 18(12), 1195-1199.

by admin | Feb 12, 2020 | Crohn's Disease, Mesenchymal Stem Cells
A recent study has shown how stem cells may be able to help Crohn’s disease patients who suffer from perianal fistulas. The researchers specifically investigated how stem cell therapy for Crohn’s Disease compared to conventional approaches including antibiotics and immunosuppressors. Because research is still in its infancy, there has been great interest in how to best address perianal fistulas in Crohn’s disease patients.
For their study, the scientists studied adults between the ages of 19 and 68. The patients were divided into three groups: one group received mesenchymal stem cell therapy applied locally, another received a combination of cellular and anti-cytokine therapy, and a third received a combination of immunosuppressors and antibiotics. The researchers looked at the impact of these three therapeutic interventions on the frequency of relapses of perianal fistulas and evaluated patients with the index of perianal activity of Crohn’s disease (PCDAI).
Their results showed that the combined cellular and anti-cytokine therapy improved perianal lesions in Crohn’s disease patients more so than did the immunosuppressor and antibiotic combination. Specifically, with the stem cell and anti-cytokine approach, fistulas remained closed longer and fistulas recurred less frequently. Future research should help to determine if and how this stem cell approach can provide an effective and safe long-term therapy for Crohn’s disease patients with perianal fistulas.
Reference: Knyazev, OV et al. (2018). Stem cell therapy for perianal Crohn’s disease. Ter Arkh, 90(3), 60-66.



 St. Petersburg, Florida
St. Petersburg, Florida
