
by admin | Jan 26, 2017 | Studies
Severe diabetics are often treated through a technique called islet transplantation, but this transplantation method has certain limitations. Researchers have recently demonstrated that that using a certain type of stem cell, called the mesenchymal stem cell, can improve the ability of islet transplants to improve diabetes in patients.
Those who suffer from Type 1 diabetes experience the destruction of beta cells in the pancreas. Islet transplantation is a means for reconstructing these cells that are lost during the progression of diabetes, but the long-term effects of traditional islet transplantation are limited, and the transplants often have to be performed a number of times on any given patient. Part of the problem is that the beta cells in the islets are easily damaged or killed once they are isolated for transplantation purposes and do not easily proliferate into other cells.
Unlike islets, mesenchymal stem cells are less vulnerable, highly proliferative, and differentiate into several cell types. They also have the added benefits of promoting healthy vasculature and immune activity. Given these benefits of mesenchymal stem cells, scientists hypothesized that combining the function of beta cells with the abilities of mesenchymal stem cells would produce a more effective therapy for diabetes than islet transplantation alone. To achieve this result, Shoichiro Sumi’s team decided to fuse these cell types together.
In a study published in PLOS One, researchers demonstrated how to successfully overcome the technical difficulty of fusing mesenchymal stem cells to islet cells for the purposes of treating diabetes. The fused cells were associated with markers that indicated that the cells were less susceptible to death than islet cells are alone and that they also proliferated more than islet cells generally do.
Having cleared the technical hurdle of fusing islet cells with mesenchymal stem cells and showing that this technique is successful in creating cells that are more robust than islet cells, researchers are now poised to test the ability of these cells to improve therapeutic interventions for those with severe diabetes. If the researchers can show that fewer transplants or longer-term results can be achieved with these fused cells, islet transplantation for diabetics may be transformed.
Learn more about how stem cells provide regenerative therapy for Diabetes here.
Reference
Yanai, G. et al (2013). Electrofusion of mesenchymal stem cells and islet cells for diabetes therapy: a rat model. PLOS One, 8(5), 1-9.

by admin | Jan 16, 2017 | Studies
In recent years, there have been a number of advances in stem cell research and in the various ways that these cells can be best employed to improve the health of patients. One of the medical areas that shows promise for stem cell therapies is orthopedics, with stem cell therapies being developed to help with tissue, cartilage, and bone repair. A recent review by Anish Majumdar and colleagues conveyed the progress that has been made specifically in the use of stem cells for the repair of cartilage in osteoarthritis.
Patients with osteoarthritis experience degeneration of their connective tissues, which progresses as they get older. While osteoarthritis is often diagnosed in older patients, athletes also often endure osteoarthritis after injuring themselves while playing sports. In osteoarthritis, tissue known as articular cartilage is particularly susceptible to injury and unfortunately does not heal as well as other tissues because it does not have the vasculature required to supply the tissue with the nutrients required for significant growth and recovery.
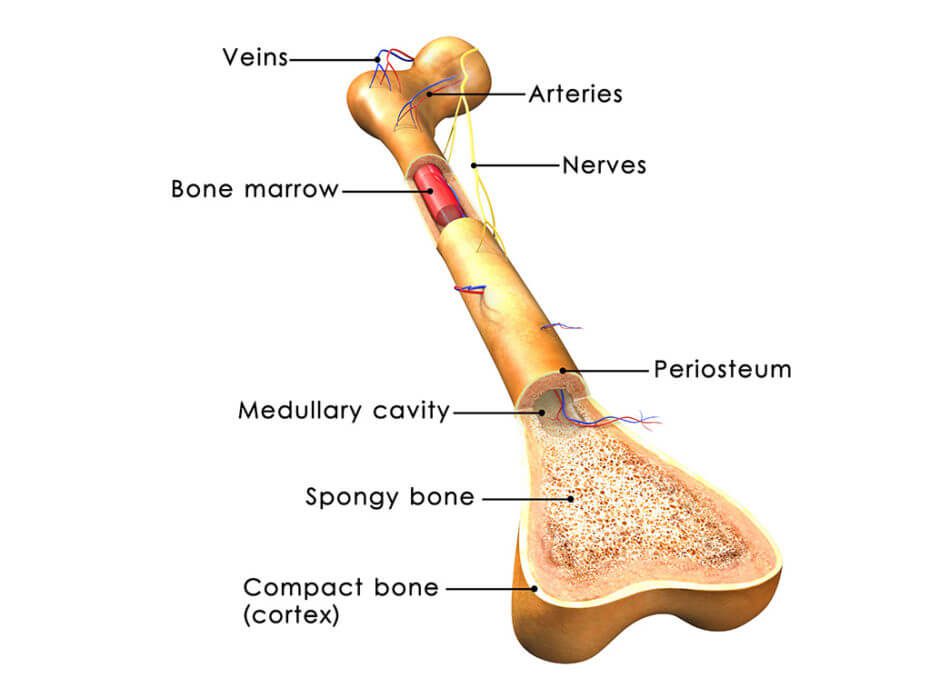
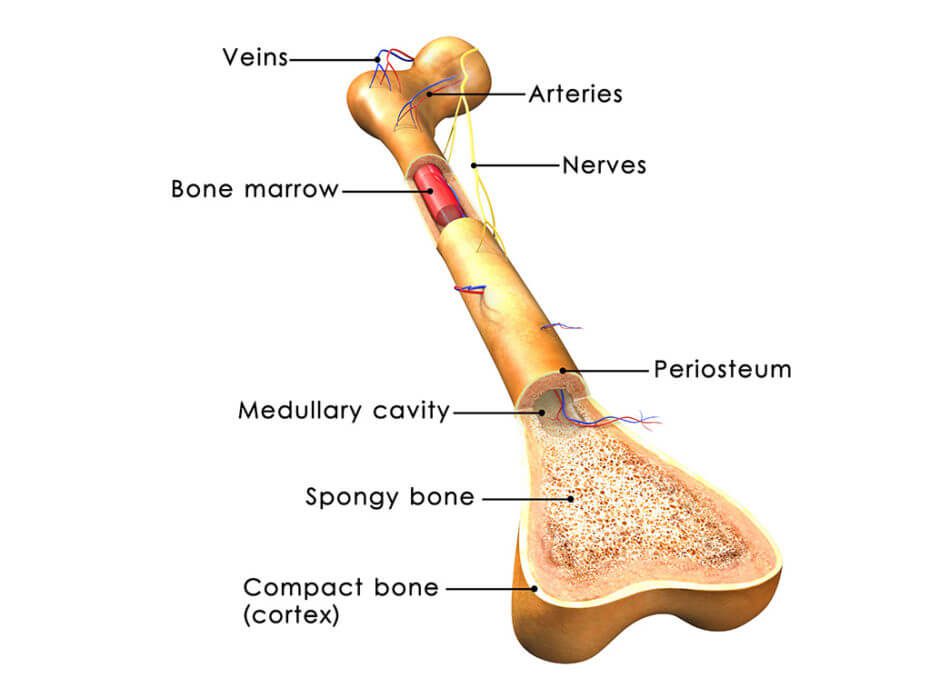
When articular cartilage is damaged, surgery is often employed in an attempt to correct the damage, and pharmaceuticals are sometimes prescribed for discomfort. However, these interventions do not tend to achieve satisfying results. Because bone marrow stromal cells, or bone marrow-derived mesenchymal stem cells, naturally differentiate into the cells that make up cartilage, it has been suggested that these stem cells could improve outcomes for those with osteoarthritis.
These particular stem cells have other advantages, including that their isolation is relatively simple and that they easily proliferate, adds to their attractiveness as a candidate for cartilage repair. Their ability to suppress the immune system and prevent inflammation makes them more likely than many other cell types to be safe when added to the cartilage. As such, according to this review, a number of researchers have reported that their injections of these stem cells in patients with osteoarthritis have not caused any problems related to safety.
These findings include stem cells leading to improvements in clinical symptoms and quality of life in those with osteoarthritis, as well as the filling of the defect area and reduction in pain.
Researchers have also reported that these stem cells are effective from a therapeutic standpoint when administered to osteoarthritis patients. A number of specific findings on the success of bone marrow-derived mesenchymal stem cells in cartilage repair demonstrate that stem cells could revolutionize therapeutic strategies for this type of tissue damage. These findings include stem cells leading to improvements in clinical symptoms and quality of life in those with osteoarthritis, as well as the filling of the defect area and reduction in pain.
See why more and more athletes are turning to stem cell therapy here.
Reference
Gupta, P.K., Das, A.K., Chullikana, A., & Majumdar, A.S. (2012). Mesenchymal stem cells for cartilage repair in osteoarthritis. Stem Cell Research & Therapy, 3(25), 1-9.

by admin | Jan 11, 2017 | Studies
A group of scientists, led by Jin Nam at the University of California-Riverside, have found a new way to optimize the use of stem cells for orthopedic purposes. The technique involves strategically using biomechanical forces to create the specific cell type needed to repair orthopedic tissues.
The normal development of bone and cartilage critically depend on mechanical stimulation, yet the ideal level of mechanical stimulation differs for cells that make up bone and cells that make up cartilage. The researchers therefore reasoned that employing the right level of mechanical stimulation could help stem cells differentiate into the cell type needed for specific individual injuries.
A certain type of stem cell, called the mesenchymal stem cell (MSC) has been shown to be capable of regenerating musculoskeletal tissues. In addition, when MSCs obtained from the patient are used to regenerate that patient’s musculoskeletal tissues, tissue rejection tends to be prevented because the immune system recognizes the transplanted cells as the body’s own cells. Nonetheless, stimulating the stem cells to form tissue has relied mainly on biochemical and biophysical phenomena, which can present a variety of challenges. To avoid those challenges, scientists hoped that they could use biomechanical stimulation for the same purpose.
In their experiment, Nam and his colleagues showed that different levels of biomechanical force could indeed lead MSCs to differentiate into osteoblasts and chondrocytes, the cells that make up bone and cartilage, respectively. These promising results suggest that combining these types of stem cells with targeted biomechanical stimuli will enable better repair of a variety of types of orthopedic damage.
Going forward, researchers hope to better understand the details of how biomechanical cues can determine the fate of stem cells and to use this information to induce stem cells to differentiate into the desired cell type, according to the particular injury. This experiment conducted at the University of California-Riverside helps shed more light on the continued value of stem cells in medicine, as well as the potential benefits of combining these cells with approaches that can help personalize the treatments offered.
Stem cells could revolutionize therapeutic strategies for cartilage repair. Find out more.
Reference
Horner, C.B. et al. (2016). Magnitude-dependent and inversely-related osteogenic/chondrogenic differentiation of human mesenchymal stem cells under dynamic compressive strain. Journal of Tissue Engineering & Regenerative Medicine. doi: 10.1002/term.2332

by admin | Jan 4, 2017 | Studies, Stem Cell Research
A specific type of stem cell called mesenchymal stem cells has shown significant promise for therapeutics against a host of diseases, and now scientists have found that they can improve the therapeutic impact of these stem cells through something called hypoxia preconditioning. They have published their findings in a journal called Cell Death and Disease.
Previous research has found that, though helpful for therapies, the effectiveness of mesenchymal stem cells is often limited by certain physiological conditions. For instance, DNA damage, cell death, and harm to tissue often persist because reactive oxygen species are produced in response to disease or injury. Insufficient nutrient levels can also minimize the therapeutic potential of mesenchymal stem cells. Studies performed to overcome these limitations by genetically modifying mesenchymal stem cells have demonstrated that this particular approach comes with its own difficulties, including toxicity and unwanted side effects.
Certain injuries lead to a shortage of blood supply to some tissue areas. When this occurs, the oxygen levels in those tissues can become severely limited in what is known as hypoxia. Hypoxia can lead to cell death and can also make it harder for stem cells to differentiate if they are applied for therapy. However, research has shown that preconditioning cells to lower oxygen level conditions can enable them to later withstand more severe hypoxia. Based on these observations, a team of scientists, led by Sang Hun Lee, hypothesized that preconditioning mesenchymal stem cells may help them survive and proliferate once they are transplanted into injured tissue.
To test their idea, the scientists preconditioned mesenchymal stem cells from people’s fat tissue to low oxygen levels and then transplanted the cells into mice whose blood supply had been cut off to certain tissues. When they compared the impact of transplanting these preconditioned cells to transplanting cells that were not preconditioned, they found that the preconditioned cells survived and proliferated at higher rates and that they were more effective in helping the mice recover functionally. These results add to the breadth of research that suggests that stem cells may have an array of therapeutic applications and that any limitations that arise may be able to be addressed by combining stem cell transplantation with other strategies.
Learn more about the benefits of stem cell therapy.
Reference
Zhao, Yan et al. (2016). Hypoxia-induced expression of cellular prion protein improves the therapeutic potential of mesenchymal stem cells. Cell Death and Disease, 7, e2395.

by admin | Nov 30, 2016 | Studies, Kidney Disease
Dr. Xun Zhu and colleagues in Rochestor, Minnesota recently reviewed the medical research that suggests that stem cells can be useful for treating kidney disease. In their review, they focused on the value of mesenchymal stem cells (MSCs), which are a type of stem cell that can turn into a number of different cell types, including bone cells, muscle cells, fat cells, and cartilage cells. MSCs have become a popular type of stem cell for therapeutic purposes for several reasons. First, they can be collected in large numbers with relative ease from places like fat tissue or bone marrow. Second, they fight inflammation, thereby reducing problematic symptoms associated with a number of diseases and conditions. Finally, MSCs seem to work along a number of different pathways that contribute to disease.
In their review, Zhu and colleagues discussed how MSCs are promising specifically within the realm of kidney disease. Both acute kidney ischemia and chronic ischemic kidney disease may be improved with MSCs and currently lack other highly effective treatment options. In addition to their anti-inflammatory properties, which can both protect and repair the kidney, MSCs also seem able to repair the kidney by releasing chemicals called cytokines. Cytokines are cells that are normally secreted by the immune system and impact other cells in ways that are important for healthy functioning.
Pre-clinical research into how MSCs may be used to address kidney disease has been promising. For instance, in a study where rat kidney transplants were being rejected by the rats’ immune systems, MSCs helped reduce the inflammation caused by the immune systems’ reactions. Similarly, in a phase II clinical trial, MSCs reduced the incidence of kidney transplant rejection in human patients. In a separate phase I clinical trial, patients who had undergone heart surgery were given injections of MSCs derived from bone marrow and as a result, were 20% less likely to suffer from acute kidney ischemia postoperatively. Further, the length of hospital stays and the readmissions rates were reduced in this group by 40%.
Researchers have also begun to consider the impact of MSCs on diabetic nephropathy, a progressive disease of the kidney that can occur in diabetes patients. Their pre-clinical studies have shown that MSCs can minimize diabetic nephropathy in rats by lowering inflammation.
The work compiled by Zhu and colleagues demonstrates that significant value that MSCs bring to treating several forms of kidney disease. Going forward, researchers will aim to determine the best route of MSC delivery for each type of disease and how long the effect of MSCs can last.
To learn more about how stem cells could help those with Diabetic kidney disease, click here.
Reference
Zhu, X.Y., Lerhman, A., & Lerman, L.O. (2013). Concise review: Mesenchymal stem cell treatment for ischemic kidney dissease. Stem Cells, 31, 1731-1736.





 St. Petersburg, Florida
St. Petersburg, Florida
