
by Shoot To Thrill Media | Oct 24, 2025 | Shoulder Pain
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified Physician
Last Updated: October 2025
Why Shoulders Hurt
Your shoulder is one of the most mobile joints in the human body, which makes it incredibly useful, but also prone to injury, strain, and degeneration.
Pain can start suddenly after an injury or gradually from overuse, inflammation, or age-related wear. It often involves tendons, cartilage, muscles, or the joint capsule itself.
Common Causes of Shoulder Pain
- Rotator cuff injuries (tendon tears or tendinopathy)
- Tendonitis or bursitis
- Shoulder impingement
- Frozen shoulder (adhesive capsulitis)
- Osteoarthritis or cartilage wear
- Labral tears
Typical Symptoms
- Persistent aching or sharp pain
- Stiffness or reduced range of motion
- Weakness or instability
- Pain at night or with overhead movement
Whether the cause is degenerative or traumatic, shoulder pain can interfere with sleep, work, and daily activities like reaching or lifting.
Conventional Treatment Options
Most providers begin with conservative care to reduce inflammation and improve function:
- Physical therapy and guided exercises
- Anti-inflammatory medications (NSAIDs)
- Corticosteroid injections for short-term relief
- Ice, heat, and stretching
- Activity modification or rest
In more advanced or chronic cases, surgical interventions may be recommended:
- Arthroscopic repair (rotator cuff or labral tears)
- Joint debridement or resurfacing
- Total shoulder replacement (for severe arthritis)
While effective, surgery can require significant recovery time and may not always restore full range of motion.
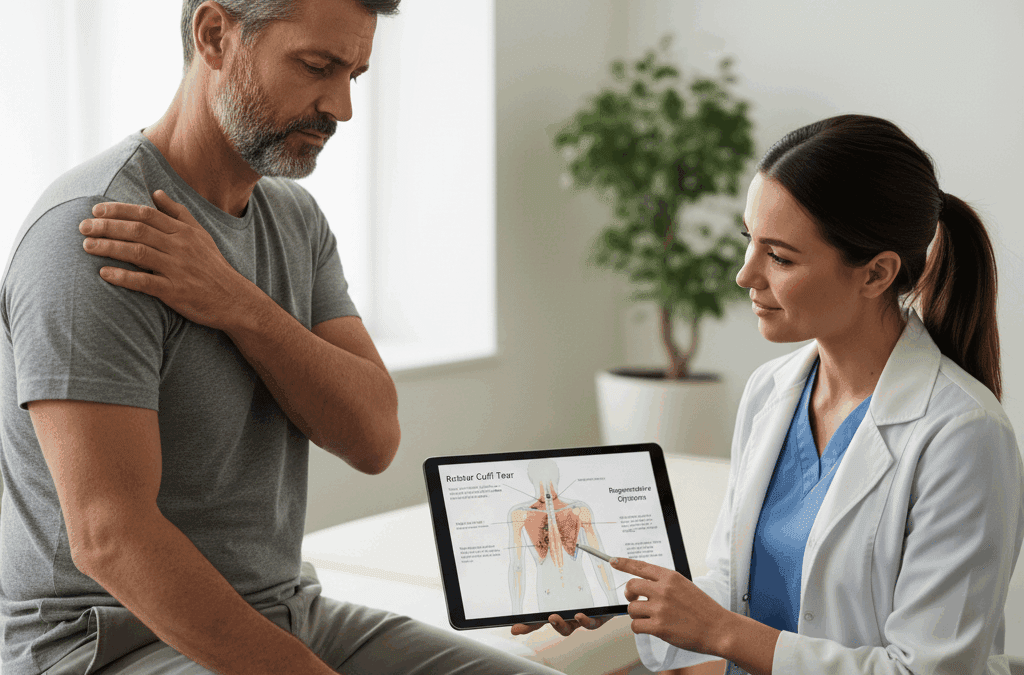
How Regenerative Therapies May Help
Regenerative medicine seeks to repair and rebuild damaged tissues rather than just masking pain.
For shoulder injuries and degenerative conditions, treatments such as stem cell therapy and platelet-rich plasma (PRP) are being explored as non-surgical options to promote natural healing.
Potential Benefits
- Reduced inflammation and tissue irritation
- Support for tendon or cartilage repair
- Improved shoulder strength and flexibility
- Faster recovery when combined with rehabilitation
- Option to delay or avoid surgery
Note: PRP and stem cell–based treatments are not FDA-approved for shoulder pain and remain investigational, but they are supported by growing clinical evidence for safety and potential benefit.
Recent Clinical Studies on Regenerative Medicine for Shoulder Pain
2024 – PRP for Frozen Shoulder: Strong Long-Term Relief
Title: “The clinical efficacy and safety of platelet-rich plasma on frozen shoulder: a systematic review and meta-analysis of randomized controlled trials”
Date: September 6, 2024
Link: Springer – BMC Musculoskeletal Disorders
Summary:
This meta-analysis of 14 RCTs (over 1,000 patients) found that PRP injections for frozen shoulder (adhesive capsulitis) significantly improved pain, range of motion, and function compared to steroid shots. PRP effects lasted longer, with no major adverse reactions reported.
2024 – PRP for Partial Rotator Cuff Tears
Title: “Comparative efficacy of platelet-rich plasma (PRP) injection versus PRP combined with vitamin C injection for partial-thickness rotator cuff tears: a randomized controlled trial”
Date: July 23, 2024
Link: Journal of Orthopaedic Surgery and Research
Summary:
Patients with partial rotator cuff tears received ultrasound-guided PRP injections. At 3 months, both PRP groups showed significant pain reduction and improved shoulder function, with no serious side effects. The study supports PRP as a safe, effective, non-surgical treatment.
2021 – Stem Cell Therapy for Tendon Disorders
Title: “Mesenchymal Stem Cells Use in the Treatment of Tendon Disorders: A Systematic Review and Meta-Analysis of Prospective Clinical Studies”
Date: August 30, 2021
Link: Annals of Rehabilitation Medicine
Summary:
This review analyzed human studies using mesenchymal stem cell (MSC) therapy, including umbilical cord tissue–derived MSCs. Results showed significant improvements in pain, tendon healing (via MRI/ultrasound), and shoulder function with no major safety issues—indicating MSCs may help restore tendon integrity in rotator cuff injuries.
2021 – PRP vs Corticosteroid for Rotator Cuff Tendinopathy
Title: “Corticosteroids or platelet-rich plasma injections for rotator cuff tendinopathy: a randomized clinical trial study”
Date: May 21, 2021
Link: Journal of Orthopaedic Surgery and Research
Summary:
In 58 patients with chronic rotator cuff tendinopathy, both PRP and steroid injections reduced pain, but PRP provided greater relief and mobility at 3 months, without the side effects associated with steroids.
2018 – PRP for Shoulder Osteoarthritis
Title: “Comparative study between platelet-rich plasma injection and steroid injection in mild–moderate shoulder osteoarthritis and their relation to quality of life”
Date: December 17, 2018
Link: Egyptian Rheumatology & Rehabilitation (SpringerOpen)
Summary:
In this 50-patient study, both groups (PRP vs. steroid) improved after treatment, but PRP resulted in greater and longer-lasting pain and function gains. The authors concluded that PRP offers durable relief without the degenerative drawbacks of repeated steroid injections.
Is Regenerative Medicine Right for You?
Regenerative therapy may be worth exploring if you:
- Have chronic shoulder pain or stiffness
- Want to avoid surgery or long recovery times
- Seek a natural approach that promotes tissue repair
- Have not found success with traditional care
At Stemedix, each treatment plan is individualized, using evidence-informed regenerative options such as PRP or MSC-derived biologics to help restore joint and tendon health under physician supervision.
Medical Disclaimer
This page is for educational purposes only and does not replace medical advice.
PRP and stem cell–based therapies for shoulder conditions are investigational and not FDA-approved.
Individual results vary; always consult a qualified medical provider.
References
- The clinical efficacy and safety of PRP on frozen shoulder: a meta-analysis. BMC Musculoskeletal Disorders, 2024.
- PRP vs. PRP + Vitamin C for partial-thickness rotator cuff tears. Journal of Orthopaedic Surgery and Research, 2024.
- Mesenchymal Stem Cells in tendon disorders: systematic review & meta-analysis. Annals of Rehabilitation Medicine, 2021.
- Corticosteroids or PRP injections for rotator cuff tendinopathy: RCT. Journal of Orthopaedic Surgery and Research, 2021.
- Comparative study between PRP and steroid injections in shoulder OA. Egyptian Rheumatology & Rehabilitation, 2018.

by Shoot To Thrill Media | Oct 23, 2025 | Rotator Cuff Injuries
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified Physician
Last Updated: October 2025
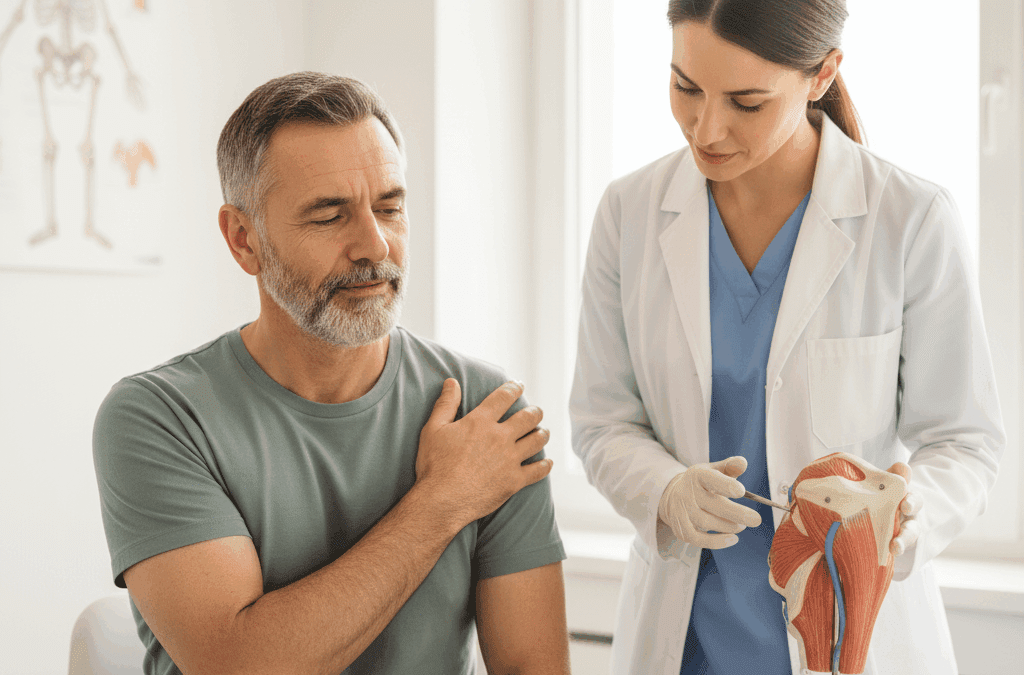
What Is a Rotator Cuff Injury?
Your rotator cuff is a group of four muscles and tendons that stabilize your shoulder and allow you to lift, reach, and rotate your arm.
Because it’s constantly in use and subject to wear, this structure is especially prone to injury — whether from overuse, degeneration, or trauma.
Common Types of Rotator Cuff Injuries
- Tendon tears (partial or complete)
- Tendonitis (inflammation from overuse)
- Impingement (tendons getting pinched between bones during movement)
Typical Symptoms
- Dull, aching shoulder pain, especially at night or when lying on the affected side
- Weakness when lifting or rotating the arm
- Clicking, catching, or grinding sensations
- Stiffness and loss of shoulder motion
Left untreated, these injuries may worsen over time, leading to chronic pain, tendon degeneration, and loss of mobility.
Conventional Treatment Options
Most rotator cuff problems are initially managed with non-surgical treatments designed to reduce inflammation and strengthen the surrounding muscles.
First-Line Therapies Often Include:
- Rest and activity modification
- Physical therapy and guided strengthening
- Ice, heat, and stretching routines
- Anti-inflammatory medications or corticosteroid injections
If symptoms persist or the tear is large, surgery may be recommended:
- Arthroscopic tendon repair
- Tendon transfer for non-repairable tears
- Shoulder replacement for severe or chronic damage
While surgery can be effective, recovery may take months and full function isn’t always restored, especially in older patients or repeat injuries.
Regenerative Medicine: A Modern Option for Shoulder Healing
Regenerative medicine offers a non-surgical approach that focuses on stimulating your body’s natural repair processes.
For rotator cuff injuries, treatments like stem cell therapy and platelet-rich plasma (PRP) are emerging as effective ways to promote tendon healing and reduce inflammation.
How These Treatments Work
- Platelet-Rich Plasma (PRP): Uses growth factors from your own blood to support tendon repair and decrease inflammation.
- Stem Cell Therapy: Uses umbilical cord tissue-derived mesenchymal stem cells (UCT-MSCs) or other sources to help regenerate damaged tendon fibers and restore strength.
- Amniotic and Perinatal Tissue Products: Contain natural healing factors and extracellular matrix proteins that support soft tissue repair.
Potential Benefits
- Decreased shoulder pain and inflammation
- Faster tendon healing and tissue remodeling
- Improved shoulder strength and range of motion
- Shorter downtime compared to surgery
- Enhanced recovery when combined with physical therapy
Note: Regenerative therapies for shoulder injuries are not yet FDA-approved and are considered investigational, but multiple peer-reviewed studies show strong safety profiles and promising results.
Recent Clinical Studies: Regenerative Medicine for Rotator Cuff Injuries
2025 – Amniotic Allograft Injections Improve Long-Term Shoulder Function
Title: Effectiveness of Amnion Allograft Injections in Patients With Degenerative Musculoskeletal Diseases
Journal: AJPMR – Full Text
Summary:
A meta-analysis of seven studies found that amniotic tissue injections (amnion allograft) significantly improved pain and mobility in patients with degenerative tendon conditions, including rotator cuff tendinopathy.
Improvements lasted months to years, and no serious adverse events were reported — confirming amniotic allografts are a safe and effective adjunct in shoulder injury management.
2024 – PRP Provides Better Long-Term Outcomes Than Steroids
Title: Subacromial PRP vs. Corticosteroid Injection for Rotator Cuff Tendinopathy: 1-Year Follow-Up
Journal: PubMed – Full Text
Summary:
In this double-blind RCT (100 patients), PRP outperformed steroid injections at the one-year mark, providing greater pain reduction and improved functional scores.
Only 12% of PRP patients required further treatment versus 30% in the steroid group, showing longer-lasting relief and fewer recurrences with PRP therapy.
2024 – PRP During Rotator Cuff Surgery Reduces Re-Tear Rates
Title: Arthroscopic Rotator Cuff Repair Combined with PRP Reduces Retear Rate: Meta-Analysis of RCTs
Journal: Medicine (LWW) – Full Text
Summary:
Analysis of 21 RCTs (1,300+ patients) found that adding PRP during surgical repair reduced tendon re-tears by ~30% and improved early postoperative shoulder function.
Researchers concluded that PRP augmentation enhances surgical outcomes by supporting better tendon healing and reducing reinjury risk.
2024 – Wharton’s Jelly Injections Show Strong Safety and Pain Relief
Title: Safety and Efficacy of Wharton’s Jelly Connective Tissue Allograft for Rotator Cuff Tears
Journal: PubMed – Full Text
Summary:
In this 87-patient study, Wharton’s Jelly (umbilical cord matrix rich in MSCs) was injected after failed conservative care.
Within 90 days, patients reported significant pain reduction and better shoulder mobility.
No adverse reactions were noted, and over 75% reported meaningful improvement — positioning Wharton’s Jelly as a promising non-surgical biologic therapy.
2023 – Umbilical Cord Tissue Therapy Shows Regenerative Potential
Title: Allogenic Umbilical Cord Tissue for Rotator Cuff Injuries: Systematic Review
Journal: PubMed – Full Text
Summary:
This review analyzed multiple lab and early clinical studies using umbilical cord tissue and MSCs in rotator cuff repair.
Findings confirmed strong safety outcomes and evidence of enhanced tendon healing.
Authors emphasized that perinatal tissue therapy holds great potential for future shoulder repair advancements.
2021 – PRP Outperforms Corticosteroids for Partial Tears
Title: PRP vs. Corticosteroid Injection in Partial-Thickness Rotator Cuff Tears
Journal: PubMed – Full Text
Summary:
In a double-blind RCT, PRP-treated patients experienced greater short-term pain reduction and shoulder function improvement at 3 months compared to steroid recipients.
Researchers concluded that PRP offers faster and more durable relief than standard cortisone shots in partial rotator cuff injuries.
Is Regenerative Medicine Right for You?
Regenerative therapy may be a good option if you:
- Have a partial rotator cuff tear or chronic tendinopathy
- Want to avoid or delay surgery
- Seek a natural, biologic option to enhance healing
- Haven’t achieved lasting relief from conventional treatments
At Stemedix, our clinicians evaluate your imaging, injury history, and activity goals to determine if regenerative medicine, such as PRP or umbilical cord tissue therapy, may be suitable for your shoulder recovery.
Medical Disclaimer
This page is intended for educational purposes only and does not replace medical evaluation or treatment.
Regenerative therapies are investigational and not FDA-approved for rotator cuff injuries.
Individual results vary. Always consult a qualified medical provider before undergoing treatment.
References
- Li J. et al. Effectiveness of Amnion Allograft Injections in Degenerative Tendon Disease. AJPMR., 2025. Full Text
- Wang T. et al. Subacromial PRP vs. Steroid for Rotator Cuff Tendinopathy. PubMed., 2024. Full Text
- Zhang P. et al. PRP Combined with Rotator Cuff Repair Reduces Retear Rate. Medicine (LWW)., 2024. Full Text
- Moreno F. et al. Wharton’s Jelly Allograft for Rotator Cuff Tears. PubMed., 2024. Full Text
- Chen H. et al. Umbilical Cord Tissue for Rotator Cuff Healing: Systematic Review. PubMed., 2023. Full Text
- Kesikburun S. et al. PRP vs. Corticosteroid in Partial Rotator Cuff Tears. PubMed., 2021. Full Text

by Shoot To Thrill Media | Oct 23, 2025 | Rheumatoid Arthritis
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified Physician
Last Updated: October 2025
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease where the body’s immune system mistakenly attacks its own joint tissue.
This inflammation primarily affects the synovial lining, the soft membrane surrounding joints, leading to pain, swelling, stiffness, and gradual cartilage and bone damage.
RA most often impacts the hands, wrists, knees, and ankles, but it can also affect the skin, eyes, lungs, and heart, making it a systemic condition.
Common Symptoms
- Swollen, tender, or warm joints
- Morning stiffness lasting 30 minutes or longer
- Fatigue or low energy
- Low-grade fever or malaise
- Symmetrical joint involvement (both sides of the body)
RA can develop slowly or suddenly and often flares in cycles of active inflammation followed by periods of remission.
Current Treatment Options
Today’s standard care focuses on slowing disease progression, reducing inflammation, and preserving joint function.
While effective for many, these treatments often require long-term use and may not fully prevent ongoing joint damage.
Commonly Used Therapies
- DMARDs (Disease-Modifying Anti-Rheumatic Drugs):
Medications such as methotrexate or leflunomide help suppress inflammation and slow joint destruction.
- Biologic agents:
Targeted drugs (like anti-TNF or IL-6 inhibitors) that block specific immune pathways.
- NSAIDs and corticosteroids:
Provide temporary relief from pain and swelling.
- Physical and occupational therapy:
Maintain joint flexibility, strength, and mobility.
- Lifestyle measures:
Anti-inflammatory diet, low-impact exercise, adequate sleep, and smoking cessation.
Although many patients benefit from these approaches, some find that medications lose effectiveness or cause side effects over time.
That’s why researchers are studying regenerative medicine as a complementary and potentially longer-lasting approach.
Regenerative Medicine: A New Approach for RA
Regenerative medicine focuses on helping the body heal and restore balance rather than only suppressing immune activity.
One of the most promising developments is the use of umbilical cord tissue-derived mesenchymal stem cells (UCT-MSCs).
How UCT-MSC Therapy May Help
These specialized cells are known for their powerful anti-inflammatory and immunomodulatory effects.
Research suggests that UCT-MSCs can:
- Calm an overactive immune system, reducing chronic inflammation in joints
- Support regeneration of damaged cartilage and joint lining
- Lower pain and swelling, promoting smoother movement
- Improve joint flexibility and potentially slow structural damage
Because these cells work by re-balancing immune signals and encouraging tissue repair, they may offer longer-term relief with fewer systemic side effects than some medications.
Note: UCT-MSC therapy for rheumatoid arthritis is investigational and not FDA-approved, but multiple clinical studies worldwide have demonstrated encouraging results regarding safety and symptom improvement.
Recent Clinical Studies in Regenerative Therapy for RA
2023 – Global Meta-Analysis Confirms Safety of MSC Therapy
Title: Safety and Efficacy of Mesenchymal Stem Cell Therapy in the Treatment of Rheumatoid Arthritis: Systematic Review and Meta-Analysis
Journal: PLOS ONE – Full Text
Summary:
A 2023 meta-analysis reviewed multiple human clinical trials using MSC therapy for RA. Results confirmed a strong safety profile, with no life-threatening events or malignancies.
Patients receiving MSCs experienced measurable reductions in joint pain and inflammation scores, suggesting a positive trend toward clinical improvement. The authors emphasized that larger randomized trials are warranted but called MSC therapy a “safe and promising immunomodulatory treatment” for RA.
2021 – Five-Year Safety Follow-Up in RA Patients
Title: Long-Term Safety of a Single Infusion of Human Umbilical Cord Blood-Derived MSCs in Rheumatoid Arthritis: Five-Year Follow-Up of a Phase I Clinical Trial
Journal: American College of Rheumatology Abstracts – Full Text
Summary:
In this extended study from South Korea, RA patients received one IV infusion of UC-MSCs. After five years, no cases of infection, clotting disorders, or cancer were reported.
Patients maintained stable immune markers and joint function without new safety concerns.
Researchers concluded that a single UC-MSC infusion is well-tolerated and safe long-term for RA patients.
2020 – UC-MSC Plus IFN-γ Greatly Improves Response Rates
Title: Combination of UC-MSC Transplantation with IFN-γ Treatment Improves Outcomes in Rheumatoid Arthritis
Journal: PubMed – Full Text
Summary:
Sixty-three patients with difficult-to-treat RA were given UC-MSCs alone or UC-MSCs combined with interferon-gamma (IFN-γ).
After three months, 93% of the combination group improved, compared to 53% in the MSC-only group.
No serious adverse events occurred.
This trial suggested that pre-activating MSCs with IFN-γ can enhance their immune-balancing effects, offering greater therapeutic benefit.
2020 – Peptide-Enhanced MSC Therapy Shows Added Benefit
Title: Cervus and Cucumis Peptides Combined with UC-MSC Therapy for RA
Journal: PMC – Full Text
Summary:
In this Chinese clinical study, patients received UC-MSC therapy either alone or combined with a natural peptide blend known for anti-inflammatory activity.
The combination group showed greater decreases in ESR, CRP, RF, and anti-CCP antibodies.
Participants also reported less joint pain and swelling after one year.
Researchers concluded that pairing regenerative therapy with bioactive peptides enhanced symptom improvement and overall disease control.
2019 – Phase I/II Trial Demonstrates Multi-Year Benefits
Title: Efficacy and Safety of UC-MSC Therapy for Rheumatoid Arthritis: Prospective Phase I/II Study
Journal: Drug Design, Development and Therapy – Full Text
Summary:
Sixty-four RA patients received one or two IV infusions of UC-MSCs alongside their standard medications.
No adverse effects on liver, kidney, or blood markers were noted.
Over 1–3 years, inflammatory biomarkers (ESR, CRP, RF, anti-CCP) decreased significantly, and disease activity scores (DAS28) improved.
Patients also reported reduced pain and disability on the HAQ scale.
Authors concluded that UC-MSC therapy used with standard RA treatments is safe, effective, and feasible for long-term management.
Could Regenerative Medicine Be Right for You?
You may consider exploring regenerative therapy if you:
- Continue to have joint pain or swelling despite DMARDs or biologics
- Are looking for a natural, cell-based alternative that targets the immune system
- Prefer a non-surgical option focused on long-term healing
- Are interested in evidence-informed, personalized care for autoimmune wellness
At Stemedix, our clinical team evaluates each patient individually to determine whether regenerative medicine could complement existing RA treatments. Our goal is to help restore balance, mobility, and a higher quality of life.
Medical Disclaimer
This content is for educational purposes only and does not replace medical advice.
Stem cell and regenerative therapies for rheumatoid arthritis are not FDA-approved and outcomes vary.
Always consult with a qualified healthcare professional before considering any investigational treatment.
References
- Liu J. et al. Safety and Efficacy of MSC Therapy in Rheumatoid Arthritis: Systematic Review. PLOS ONE., 2023. Full Text
- Wang D. et al. Five-Year Safety of UC-MSC Infusion in RA. ACR Abstracts., 2021. Full Text
- Yang X. et al. UC-MSC and IFN-γ Combination Therapy in RA. PubMed., 2020. Full Text
- Zhang L. et al. Cervus & Cucumis Peptides with UC-MSCs for RA. PMC., 2020. Full Text
- Wang L. et al. Efficacy and Safety of UC-MSC Therapy in RA Patients. DDDT., 2019. Full Text

by Shoot To Thrill Media | Oct 23, 2025 | Lupus
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified Physician
Last Updated: October 2025
What Is Lupus?
Lupus is a chronic autoimmune disease that can affect nearly any organ in the body.
When the immune system, which normally protects against infection, starts attacking healthy tissues, widespread inflammation and tissue damage can occur.
The most common form is Systemic Lupus Erythematosus (SLE).
Because lupus can look different from person to person, symptoms may range from mild fatigue to severe organ involvement.
Common Symptoms Include:
- Joint or muscle pain
- Fatigue or “flu-like” malaise
- Butterfly-shaped rash across the cheeks or nose
- Sensitivity to sunlight
- Fever, hair loss, or mouth ulcers
- In more advanced cases, kidney, heart, lung, or nervous-system inflammation
People often experience flares, periods when symptoms worsen, followed by times of remission when symptoms ease.
Traditional Treatment Options
Current lupus care focuses on reducing inflammation, controlling symptoms, and preventing organ damage.
Common approaches include:
- Anti-inflammatory medications (NSAIDs) for pain and swelling
- Corticosteroids to control flares
- Immunosuppressants (e.g., azathioprine, mycophenolate, cyclophosphamide)
- Biologic therapies targeting specific immune pathways (such as belimumab or anifrolumab)
- Lifestyle management: stress reduction, sun protection, and gentle exercise
While these therapies can help many patients, some continue to experience flares or medication side effects, and complete disease control may remain challenging.
How Regenerative Medicine Could Help
Regenerative medicine introduces a new perspective for patients living with autoimmune conditions like lupus.
Rather than simply suppressing the immune system, umbilical-cord-derived mesenchymal stem cells (UCT-MSCs) aim to rebalance it.
Potential Benefits of UCT-MSCs in Lupus:
- Calm overactive immune responses by reducing inflammatory cytokines
- Encourage regulatory immune cells, helping restore balance instead of total suppression
- Release trophic and anti-inflammatory factors that aid in tissue repair
- Potentially reduce disease flares and support long-term stability
In research settings, UCT-MSCs have been shown to be well-tolerated, and some studies suggest they can improve disease activity and quality of life in patients with moderate to severe lupus.
Important:
MSC-based regenerative therapies for lupus are investigational and not FDA-approved.
They are being studied as adjunctive options for patients who have not responded fully to conventional care.
Recent Clinical Studies of Regenerative Stem Cell Therapy for Lupus
2025 – Double-Blind RCT Using MSC Secretome
Title: Umbilical Cord MSC-Derived Secretome as a Potential Treatment for SLE: A Double-Blind Randomized Controlled Trial
Journal: Stem Cell Research & Therapy – Full Text
Summary:
Twenty-nine women with active lupus received weekly injections of MSC-secretome (the bioactive solution produced by MSCs) or placebo for six weeks.
Patients receiving MSC-secretome had significant reductions in lupus disease activity scores and improved immune markers such as complement C3 and lower inflammatory cytokines (IL-6, TNF-α).
The treatment was safe and well-tolerated, with no severe adverse events.
2025 – Meta-Analysis Across Autoimmune Diseases (Including Lupus)
Title: Efficacy and Safety of MSC Transplantation in Autoimmune and Rheumatic Diseases
Journal: Stem Cell Research & Therapy – Full Text
Summary:
This large review analyzed 42 randomized trials (2,183 patients).
In lupus subgroups, MSC therapy significantly lowered SLE Disease Activity Index (SLEDAI) scores (SMD ≈ –2.32, p=0.0003).
No increase in adverse events was found versus controls.
Researchers concluded MSC therapy is safe and shows measurable improvement in lupus disease activity.
2024 – Phase 1 Dose-Escalation Trial in France
Title: Allogeneic UC-MSC Therapy for Refractory Lupus: A Phase 1 Study
Journal: PubMed Central – Full Text
Summary:
Eight patients with severe, treatment-resistant lupus received escalating doses of UC-MSCs (2–4 million cells/kg).
Treatment was well-tolerated, with only mild transient infusion reactions in two participants.
Over a year of follow-up, disease activity stabilized or improved, supporting safety even at higher doses.
2022 – Phase 1 UC-MSC Trial for Refractory SLE
Title: Safety, Immunologic Effects, and Clinical Response of UC-MSCs in SLE
Journal: Frontiers in Immunology – Full Text
Summary:
Six patients with active lupus unresponsive to medication received a single UC-MSC infusion (1×10⁶ cells/kg).
By 24 weeks, 83% achieved the lupus responder endpoint (SRI-4), showing reduced disease activity and normalization of B-cell profiles.
No serious side effects occurred.
The trial concluded UC-MSC infusion was safe and associated with meaningful clinical improvement.
Could This Be the Right Option for You?
You may wish to explore regenerative options if you:
- Have systemic or cutaneous lupus that remains active despite standard therapy
- Experience recurrent flares or medication intolerance
- Want to learn about immune-modulating, research-based alternatives that may complement current care
At Stemedix, we focus on patient-centered regenerative medicine backed by emerging clinical evidence. Our team reviews your medical history, current treatment, and goals to determine whether regenerative medicine approaches could be a safe adjunctive path forward.
Medical Disclaimer
This page is for educational purposes only and does not constitute medical advice.
Stem cell and secretome-based treatments for lupus are not FDA-approved, and outcomes vary by individual.
Always consult a licensed rheumatologist or qualified healthcare provider before making treatment decisions.
References
- Al-Shaer A. et al. Umbilical Cord MSC-Derived Secretome in SLE. Stem Cell Res Ther., 2025. Full Text
- Chen Y. et al. MSC Therapy in Autoimmune and Rheumatic Diseases: Meta-Analysis. Stem Cell Res Ther., 2025. Full Text
- Dubois M. et al. Allogeneic UC-MSC Treatment for SLE: Phase 1 Trial. PubMed, 2024. Full Text
- He L. et al. Safety and Immune Response of UC-MSCs in Refractory SLE. Front Immunol., 2022. Full Text

by Shoot To Thrill Media | Oct 23, 2025 | Knee Injuries
Medical Review: Dr. Gerald Mastaw, MD – Board-Certified Physician
Last Updated: October 2025
Why Knee Pain Happens
Your knee joint is one of the body’s most complex and hard-working joints — where your thighbone (femur), shinbone (tibia), and kneecap (patella) meet, supported by strong ligaments, tendons, and cartilage.
Because it absorbs so much pressure during daily movement, it’s also one of the most commonly injured joints.
Common Knee Problems Include:
- Ligament injuries such as ACL, MCL, or PCL tears
- Meniscus tears (cartilage cushion damage)
- Cartilage degeneration or osteoarthritis
- Tendon strains or partial tears
- Fractures or post-surgical pain
Typical Causes
- Sudden impact or twisting during sports
- Repetitive stress from daily activity
- Gradual wear-and-tear with age
- Falls, trauma, or prior surgery
When your knee is injured or inflamed, symptoms can include:
- Sharp or aching pain
- Swelling and stiffness
- Locking, catching, or popping
- Weakness or instability
- Pain that worsens with walking, stairs, or sitting
Traditional Treatment Options
Conventional treatments are designed to reduce pain and inflammation, allowing the body to heal naturally or prepare for surgery if needed.
First-Line Treatments Often Include:
- Rest, Ice, Compression, Elevation (RICE)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Physical therapy and strengthening exercises
- Knee braces or sleeves for joint support
- Activity modification and weight management
Surgical Options (for Severe Damage):
- Arthroscopy to remove or repair damaged tissue
- Ligament reconstruction (ACL, MCL, or meniscus repair)
- Cartilage restoration procedures
- Partial or total knee replacement
While effective, these procedures can involve long recovery times and may not fully restore natural joint tissue.
Regenerative Medicine: A New Approach to Knee Repair
Rather than simply managing symptoms, regenerative medicine focuses on stimulating your body’s own healing processes.
The goal is to repair and restore damaged tissues, not just mask pain.
1. Stem Cell Therapy
- Uses the body’s own repair cells, or donor umbilical cord tissue-derived mesenchymal stem cells (UCT-MSCs), to promote regeneration.
- Cells are processed under sterile, compliant conditions and injected directly into the knee.
- May help repair cartilage, tendons, and ligaments while reducing inflammation.
2. Platelet-Rich Plasma (PRP) Therapy
- Uses concentrated platelets and growth factors from your own blood.
- Delivered directly into the joint or injury site.
- Supports natural healing, inflammation control, and tissue remodeling.
Reported Benefits (Based on Clinical Studies):
- Reduced pain and swelling
- Improved flexibility and joint movement
- Enhanced recovery time after injury
- Minimally invasive, with little to no downtime
- May help delay or avoid knee replacement
Note: Stem cell and PRP therapies are not yet FDA-approved for knee osteoarthritis or injury. They remain investigational, but growing clinical evidence supports their safety and potential efficacy.
Recent Clinical Studies on Regenerative Therapies for Knee Conditions
2025 – UC-MSC Exosomes Reduce Inflammation and Support Cartilage Repair
Title: Injection of Human Umbilical Cord Mesenchymal Stem Cell Exosomes for the Treatment of Knee Osteoarthritis
Journal: PMC – Full Text
Summary:
Patients with knee osteoarthritis received intra-articular injections of umbilical cord-derived MSC exosomes (healing vesicles).
All participants tolerated treatment well with no major side effects. MRI scans and clinical scores showed less inflammation and improved cartilage quality, confirming that UC-MSC exosomes safely support cartilage regeneration.
2025 – PRP Combined with HA Reduces Bone Inflammation
Title: Clinical Efficacy of PRP and Hyaluronic Acid vs. HA Alone for Knee Osteoarthritis
Journal: MDPI – Journal of Clinical Medicine – Full Text
Summary:
In this Singapore trial (58 knees), patients received either HA alone or HA + PRP.
Both improved pain and function, but the PRP+HA group had less bone marrow inflammation on MRI at 12 months, suggesting enhanced joint protection and tissue stability with PRP supplementation.
2025 – Umbilical Cord Stem Cell Injection Outperforms Steroid Treatment
Title: Efficacy of a Single Dose of Cryopreserved UC-MSCs vs. Corticosteroid Injection for Knee OA
Journal: PubMed – Full Text
Summary:
Thirty patients were randomized to receive either a single UC-MSC injection (CellistemOA) or a steroid injection.
After one year, the UC-MSC group had greater improvements in pain, stiffness, and mobility, with no adverse events.
Researchers concluded that UC-MSC therapy was both safe and superior to corticosteroids for symptom relief in knee OA.
2024 – HA + Growth Hormone + Stem Cells Improve Function
Title: Evaluating Synergistic Effects of HA, UC-MSCs, and Growth Hormones in Knee Osteoarthritis
Journal: MDPI – Biomedicines – Full Text
Summary:
Fifty-one patients were treated with different combinations of HA, UC-MSCs, and growth hormone.
All groups reported significant pain and function improvement (WOMAC and VAS scores) at 12 months, with no major safety issues.
Although cartilage regrowth on MRI was limited, the combined regenerative therapy safely improved mobility and comfort.
2023 – PRP Meta-Analysis Confirms Pain Reduction
Title: Efficacy and Safety of PRP for Osteoarthritis: Systematic Review and Meta-Analysis
Journal: Frontiers in Medicine – Full Text
Summary:
Across 24 randomized trials (1,344 patients), PRP significantly reduced pain and improved knee function compared to other non-surgical treatments.
The authors concluded that PRP therapy “can safely and effectively improve functional activity in patients with knee OA.”
2023 – Repeated UC-MSC Injections Improve Function
Title: Repeated Intra-Articular Injections of Umbilical Cord MSCs for Knee Osteoarthritis: Phase I Trial
Journal: PMC – Full Text
Summary:
Fourteen patients received weekly UC-MSC knee injections for four weeks.
All participants reported significant pain reduction (VAS: 6.0 → 3.5) and better function (WOMAC: 26.0 → 8.5) with no serious adverse effects.
Researchers found that repeated UC-MSC therapy was safe, well-tolerated, and led to consistent improvements across all subjects.
Could Regenerative Therapy Be Right for You?
Regenerative medicine may be worth considering if you:
- Have chronic knee pain unrelieved by standard care
- Are managing osteoarthritis, meniscus tears, or ligament injuries
- Want to delay or avoid joint replacement
- Prefer a non-surgical, biologic approach to healing
Best Candidates Often Have:
- Realistic expectations and a willingness to follow rehab protocols
- Stable general health
- Commitment to maintaining post-treatment mobility and joint care
At Stemedix, our clinicians develop customized regenerative care plans that may include PRP, MSCs, or combined therapies, all grounded in scientific research and delivered under physician supervision.
Medical Disclaimer
This page is for educational purposes only and does not replace medical advice.
Stem cell and PRP therapies are investigational and not FDA-approved for knee pain or osteoarthritis.
Outcomes vary between individuals. Always consult a qualified healthcare provider before undergoing treatment.
References
- Wu J. et al. UC-MSC Exosomes for Knee OA. PMC., 2025. Full Text
- Tan S. et al. PRP + HA vs. HA for Knee OA. J Clin Med., 2025. Full Text
- Medina R. et al. Cryopreserved UC-MSCs vs. Steroid for Knee OA. PubMed., 2025. Full Text
- Rahman A. et al. HA + UC-MSCs + GH in Knee OA. Biomedicines., 2024. Full Text
- Zhang Y. et al. PRP for Osteoarthritis: Systematic Review. Front Med., 2023. Full Text
- Lee H. et al. Repeated UC-MSC Injections for Knee OA. PMC., 2023. Full Text


 St. Petersburg, Florida
St. Petersburg, Florida
