
by admin | Sep 29, 2017 | Stem Cell Research
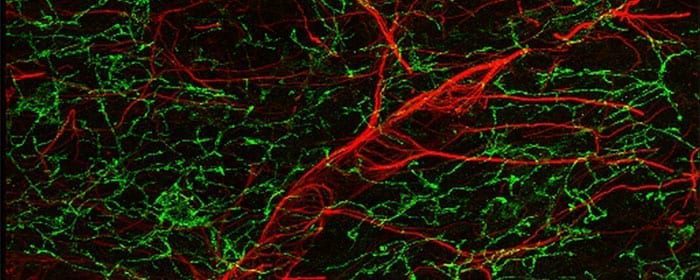
A recent review published in BMC Neuroscience synthesizes research related to intranasal delivery and describes comprehensively how the method targets therapeutic agents to the central nervous system to treat neurodegenerative disease. Perhaps the most critical aspect of intranasal delivery is that it bypasses the blood-brain barrier, a barrier that limits the ability of other therapeutic approaches to successfully impact the brain and spinal cord.
According to the researchers, other advantages of intranasal delivery include its non-invasive nature and its rapid action. Intranasal delivery causes less pain and distress than other procedures, such as brain surgery, that are used to intervene in central nervous system activity when the blood-brain barrier cannot be penetrated with other available techniques. Further, intranasal delivery delivers drugs to the central nervous system in just minutes.
Given that intranasal administration is a relatively new approach, much research must be conducted to confirm which therapies can be effectively delivered to the central nervous system with this approach, as well as which diseases can be successfully treated with the method. Basic science research has provided promising data for the use of intranasal administration to reverse neurodegeneration and to rescue memory in Alzheimer’s disease. Specific molecules have also been shown to protect the brain against stroke, as well as to stimulate the formation of new brain cells.
Research in Alzheimer’s patients and those with mild cognitive impairment has shown that intranasal insulin can improve memory and attention. Intranasal insulin has also been shown to enhance memory and mood in normal adults who do not suffer from clinical neurodegeneration. As more studies are performed on intranasal administration, it is likely that new uses of the technique will arise. Molecules, for instance, that have not yet been tested could become promising candidates for treating neurological disorders, and interventions for diseases that have not yet been adequately explored in terms of the relevance of intranasal administration may be developed.
Learn more about Alzheimer’s disease treatment here.
Reference
Hanson, LR, & Frey, WH. (2008). Intranasal delivery bypasses the blood-brain barrier to target therapeutic agents to the central nervous system and treat neurodegenerative disease. BMC Neuroscience, 9(3), 55-59.

by admin | Sep 27, 2017 | Osteoarthritis
In a review published in Stem Cell Research & Therapy, Gupta et al. describe the latest advances in the use of bone marrow derived stem cells to treat osteoarthritis. These cells are promising because of their ability to treat the degeneration of cartilage that occurs in the disease. When connective tissue degenerates, natural regeneration is highly limited because there is not a strong presence of vasculature within that tissue. Thus, interventions to deal with the effects of osteoarthritis are needed.
Historically, non-stem cell treatments have been used in attempts to treat cartilage degeneration. Physical therapy, pharmaceuticals, and surgical interventions have all been largely employed. For mild cases of osteoarthritis, combinations of physical therapy and pharmaceuticals have been used to manage pain and minimize inflammation. Unfortunately, because the disease is progressive, this type of approach is only effective in the short-term.
Eventually, steroids or hyaluronic acid are generally used to treat osteoarthritis. The impact of these more aggressive treatments, however, is debated and does not appear to be consistent across patient populations. Once osteoarthritis reaches the advanced stage, joint replacement is the only option for relief.
The use of cell-based therapies to treat osteoarthritis is not a new idea. Cultured autologous chondrocytes have been shown to successfully treat cartilage degeneration for over 15 years. The downsides to this approach are that it is invasive, the positive effects are likely temporary, and there has not been sufficient research conducted to fully understand how well the technique works and how to optimize it.
Bone marrow derived stem cells have the potential to carry the same success rate as the cell-based therapies that have long been used to treat osteoarthritis while also overcoming the limitations of those therapies. There are several advantages of the application of bone marrow derived stem cells in the treatment of cartilage degeneration.
First, these particular cells can be easily isolated. Second, they can significantly expand in culture before being used therapeutically. Third, they have modulatory properties that enable them to reduce inflammation, which is a critical factor in cartilage degeneration. Finally, they secrete factors that have the potential to both prevent further degeneration and facilitate regeneration.
Given the number of reasons that bone derived stem cells should theoretically improve upon current methods for treating the cartilage degeneration that occurs in osteoarthritis, more research will likely be conducted to decipher whether these cells do indeed provide benefits that other treatment options do not. In the case that these cells continue to appear promising for osteoarthritis treatment, research will likely also aim at determining the best protocols for using these cells to ensure the best outcomes for osteoarthritis patients.
To find out more about the new alternative way to manage the symptoms of Osteoarthritis, click here.
Reference:
Gupta, PK, Das, AK, Chullikana, A, & Majumdar, A. (2012). Mesenchymal stem cells for cartilage repair in osteoarthritis. Stem Cell Research & Therapy, 3, 25-34.

by admin | Aug 7, 2017 | Studies
A recent review in the World Journal of Stem Cells has described the nature of umbilical cord-derived mesenchymal stem cells and the clinical advantages of using these stem cells over other types of stem cells. Other mesenchymal stem cells that are used in research come from: bone marrow, peripheral blood, cord blood, placenta, adipose tissue, dental pulp, and fetal liver and lungs.
One of the main advantages of umbilical cord stem cells, for both research and clinical purposes, is its ease of collection. The collection is noninvasive, circumventing the issue of causing pain to extract the cells. Further, as umbilical cord is generally viewed as medical waste, the cells can be collected without the same ethical issues that are raised by the collection of other cell types.
The cells are also plentiful when collected and can be banked for later use. According to the researchers, the only disadvantage of umbilical cord stem cells in this context is that a physician must evaluate the baby donor’s health and confirm that the cells derive from a healthy baby. This requirement stems from the fact that the cells are more likely to develop into healthy cells themselves if they come from a healthy baby. However, in the case of bone marrow-derived mesenchymal stem cells, a physician can evaluate the potential donor first and then decide whether to collect the cells.
The immunomodulatory characteristics of umbilical cord-derived mesenchymal stem cells also represent a major practical advantage of these cells for clinical applications. The introduction of any foreign agent to the body poses a risk because the immune system may recognize the matter as foreign and deem it threatening. If this immune response occurs, the immune reaction that ensues can cause severe long-term damage to tissues. Given that umbilical cord-derived mesenchymal stem cells cause these immune reactions much less frequently than do other stem cell types makes them potentially safer as therapeutic interventions.
More research is needed to determine the best ways to use umbilical cord-derived mesenchymal stem cells. However, the evidence that there are clinical benefits to using these cells over other stem cell types is accumulating.
To learn more about the five benefits of stem cell therapy, click here.
Reference
Nagamura-Inoue & He, H. (2014). Umbilical cord-derived mesenchymal stem cells: Their advantages and potential clinical utility. World Journal of Stem Cells, 6(2), 195-202.

by admin | Aug 1, 2017 | Studies
A recent study, published in the Journal of Clinical Oncology, demonstrates that the repeated infusion of mesenchymal stem cells could improve the safety of certain type of stem cell cancer therapies. Specifically, this approach could reduce dangerous graft-versus-host disease (cGVHD) symptoms in patients who have undergone a certain type of stem cell transplantation, known as HLA-haploidentical hematopoietic stem-cell transplantation (HLA-haplo HSCT).
While HLA-haplo HSCT can reduce the risk of relapse in leukemia patients, it is also associated with an immune reaction that is the leading cause of death in the patients that do not relapse. In these cases, the patient’s immune system mistakes the newly transplanted stem cells as dangerous foreign agents and attacks them. This reaction leads to organ damage and death.
Given that HLA-haplo HSCT can be effective against leukemia, researchers have wanted to find a way to increase its safety. This study was undertaken to determine if multiple infusions of mesenchymal stem cells could help the immune system learn to cope with the stem cells and minimize their reaction.
To test their idea, researchers studied 124 patients who had undergone HLA-haplo HSCT. They gave half of those patients multiple infusions of mesenchymal stem cells, and the other half received saline infusions known to have no effect. The researchers found that the patients who were given the mesenchymal stem cell infusions had a lower incidence of cGVHD than the patients who were given saline infusions.
Not only were the symptoms different between the group who received mesenchymal stem cell infusions and those who did not, but so too was the activity of immune cells. The mesenchymal stem cell infusions resulted in more memory B lymphocytes and regulatory T cells, both of which could help mitigate cGVHD symptoms. These infusions were also associated with fewer natural killer cells, which are important cells for immune cell reactions like cGVHD.
While more research is needed to determine exactly how mesenchymal stem cells should be used to prevent cGVHD and to what extent these cells can improve the safety of HLA-haplo HSCT, these results provide hope that leukemia patients will be able to more safely receive effective stem cell treatments in the future.
To learn more about the safety of adipose stem cell procedure, click here.
Reference
Gao et al. (2016). Phase II multicenter, randomized, double-blind controlled study of efficacy and safety of umbilical cord-derived mesenchymal stromal cells in the prophyalxis of chronic graft-versus-host disease after HLA-haploidentical stem cell transplantation. Journal of Clinical Oncology, 34(24), 2843-2853.

by admin | Jul 5, 2017 | Studies
Research has long shown that nitric oxide regulates the cardiovascular system. The molecule naturally occurs within cells and organs of the body but quickly degrades. Physicians and scientists have therefore suggested that supplementing patients with cardiovascular issues with nitric oxide could be beneficial. Recently, studies have shown that this type of nitric oxide supplementation does indeed improve blood pressure and other cardiovascular functions.
Two recent studies specifically employed an orally disintegrating lozenge that supplements the body with nitric oxide through the oral cavity. One of these studies was performed on 30 patients with clinical hypertension, and the other was performed on 30 patients with pre-hypertension. Whereas hypertension refers to chronically high blood pressure, prehypertension is a clinical stage that leads to this condition. Previously, the only treatment options for prehypertension were changes to diet and lifestyle.
The impact of the nitric oxide supplementation was seen with a single dose for hypertensive patients and observed after a 30-day period of supplementation in the pre-hypertensive patients. In both groups, the oral supplements reduced blood pressure. In the hypertensive patients, the lozenges also improved endothelial function and vascular compliance in patients who were not otherwise treated for hypertension. Endothelial function refers to the functioning of the inner lining of the blood vessels, whereas vascular compliance refers to how well the arteries and veins stretch when exposed to pressure. In the pre-hypertensive patients, functional capacity was also improved, as was quality of life. The quality life measure was not assessed in the hypertensive patients but may too have been improved.
Unlike many medical interventions, nitric oxide supplementation has counterparts that naturally occur in the human body. Given that it is already present in the body, it is reasonable to assume that nitric oxide, at least at certain doses, is safe. This new literature that demonstrates the beneficial cardiovascular effects of nitric oxide supplementation suggests that nitric oxide supplements may represent a promising new therapeutic intervention in cardiovascular medicine.
References
- Biswas, O.S., Gonzalez, V.R., & Schwarz, E.R. (2014). Effects of an oral nitric oxide supplement on functional capacity and blood pressure in adults with prehypertension. Journal of Cardiovascular Pharmacology and Therapeutics, 1-7.
- Houston, M, & Hays, L. (2014). Acute effects of an oral nitric oxide supplement on blood pressure, endothelial function, and vascular compliance in hypertensive patients. Journal of Clinical Hypertension, 1-6.

 St. Petersburg, Florida
St. Petersburg, Florida
