
by admin | Oct 14, 2017 | Stem Cell Research
Research into stem cell-based therapies has increased in recent years due to observations that these types of cells can provide new avenues for treatment where other treatment options are limited. Though bone marrow mesenchymal stem cells have been the gold standard of stem cell-based therapies, there is mounting evidence that umbilical cord stem cells may offer some advantages over bone marrow mesenchymal stem cells, as well as other popular stem cell types, such as adipose tissue, periodontal ligament, and dental pulp. In a recent review in Tissue Engineering, Reine El Omar and colleagues describe the state of umbilical cord stem cell research and the potential benefits of using these cells in stem cell therapies.

According to Omar et al., umbilical cord-derived stem cells were once thought of as medical waste. However, they have now been shown to provide advantages over other stem cells in stem cell-based therapies in 3 major ways:
- Umbilical cord stem cells are easier to collect than are other stem cell types. Extracting bone marrow mesenchymal stem cells, for instance, is technically difficult and painful for donors. Umbilical cord stem cells can be painlessly collected and banked.
- Stem cells tend to proliferate more than other stem cells types. Other stem cell types have been shown to have limited proliferation and differentiation potential. Umbilical cord stem cells, on the other hand, appear to be more proliferative and differentiate longer.
- Umbilical cord stem cells are associated with less severe immune reactions than are other stem cells types. A critical aspect of the practicality of stem cells is their ability to act as therapeutic agents without causing adverse reactions. When the immune system perceives stem cells as dangerous foreign agents, the immune system can react in dangerous ways that lead to tissue damage and even death. Compared to other types of stem cells, umbilical cord stem cells appear to be associated with less severe immune reactions.
While efficacy is important for stem cell-based therapies, safety is perhaps more critical. Thus, research into how stem cells can be used therapeutically must focus not only on what therapeutic impact these cells can have but also what risks these cells pose. Future research will help to determine the safest cells to use and how those cells can best be incorporated to achieve their therapeutic goals.
Learn more about stem cell treatments here.
Reference
Omar et al. (2014). Umbilical cord mesenchymal stem cells: The new gold standard for mesenchymal stem cell-based therapies?

by admin | Sep 29, 2017 | Stem Cell Research
A recent review published in BMC Neuroscience synthesizes research related to intranasal delivery and describes comprehensively how the method targets therapeutic agents to the central nervous system to treat neurodegenerative disease. Perhaps the most critical aspect of intranasal delivery is that it bypasses the blood-brain barrier, a barrier that limits the ability of other therapeutic approaches to successfully impact the brain and spinal cord.
According to the researchers, other advantages of intranasal delivery include its non-invasive nature and its rapid action. Intranasal delivery causes less pain and distress than other procedures, such as brain surgery, that are used to intervene in central nervous system activity when the blood-brain barrier cannot be penetrated with other available techniques. Further, intranasal delivery delivers drugs to the central nervous system in just minutes.
Given that intranasal administration is a relatively new approach, much research must be conducted to confirm which therapies can be effectively delivered to the central nervous system with this approach, as well as which diseases can be successfully treated with the method. Basic science research has provided promising data for the use of intranasal administration to reverse neurodegeneration and to rescue memory in Alzheimer’s disease. Specific molecules have also been shown to protect the brain against stroke, as well as to stimulate the formation of new brain cells.
Research in Alzheimer’s patients and those with mild cognitive impairment has shown that intranasal insulin can improve memory and attention. Intranasal insulin has also been shown to enhance memory and mood in normal adults who do not suffer from clinical neurodegeneration. As more studies are performed on intranasal administration, it is likely that new uses of the technique will arise. Molecules, for instance, that have not yet been tested could become promising candidates for treating neurological disorders, and interventions for diseases that have not yet been adequately explored in terms of the relevance of intranasal administration may be developed.
Learn more about Alzheimer’s disease treatment here.
Reference
Hanson, LR, & Frey, WH. (2008). Intranasal delivery bypasses the blood-brain barrier to target therapeutic agents to the central nervous system and treat neurodegenerative disease. BMC Neuroscience, 9(3), 55-59.

by admin | Apr 27, 2017 | Stem Cell Research
Stem cells have shown promise for treating a number of autoimmune diseases, where the immune system attacks the body. Lupus causes chronic inflammation as a result of immune system attack of the body’s tissues and organs and so is a reasonable candidate for stem cell therapy.
The cells of the immune system that tend to be attacked in lupus are bone marrow cells, so replacing these cells with stem cells could improve the inflammation that occurs in the disease. Recent research has shown that stem cells do in fact demonstrate an ability to help with lupus-like diseases. A recent paper published in Experimental Nephrology described the development of this research and some of the results.
The scientists who authored this recent paper had previously shown that bone marrow transplantation could be used to reconstruct the immune system in a way that could cure severe immunodeficiency, as well as other fatal diseases including forms of cancer and congenital abnormalities due to genetic disorders or problems with metabolism.
More recently, they have begun conducting stem cells transplants with a specific stem cell type called hematopoietic stem cells. These cells have been successfully used in oncology to treat cancers, and it was hypothesized that they could also be useful in autoimmune diseases like lupus.
An advantage to using these cells is that much of the work had already been done to determine how to best isolate the stem cells and how to perform transplantations with them. It is therefore not surprising that researchers successfully transplanted these cells during their research into the application of these cells in lupus-like diseases. Their results showed that hematopoietic stem cells could both prevent and cure a host of autoimmune problems that are related to lupus.
Though hematopoietic stem cell transplantation has been performed on patients since 1997 and is conducted in parts of Europe, as well as in China and Brazil, clinical trials in the United States are still underway. Further research will help to define the specific role of hematopoietic stem cells in potential treatment options for lupus and related diseases and to determine how to safely deploy these strategies.
Stem cell treatment for lupus is a new alternative therapy to help manage the symptoms of this disease. Learn more about it here.
Reference
Good, RA et al. (2002). Mixed bone marrow or mixed stem cell transplantation for prevention or treatment of lupus-like diseases in mice. Experimental Nephrology, 10(5-6), 408-420.

by admin | Jan 4, 2017 | Studies, Stem Cell Research
A specific type of stem cell called mesenchymal stem cells has shown significant promise for therapeutics against a host of diseases, and now scientists have found that they can improve the therapeutic impact of these stem cells through something called hypoxia preconditioning. They have published their findings in a journal called Cell Death and Disease.
Previous research has found that, though helpful for therapies, the effectiveness of mesenchymal stem cells is often limited by certain physiological conditions. For instance, DNA damage, cell death, and harm to tissue often persist because reactive oxygen species are produced in response to disease or injury. Insufficient nutrient levels can also minimize the therapeutic potential of mesenchymal stem cells. Studies performed to overcome these limitations by genetically modifying mesenchymal stem cells have demonstrated that this particular approach comes with its own difficulties, including toxicity and unwanted side effects.
Certain injuries lead to a shortage of blood supply to some tissue areas. When this occurs, the oxygen levels in those tissues can become severely limited in what is known as hypoxia. Hypoxia can lead to cell death and can also make it harder for stem cells to differentiate if they are applied for therapy. However, research has shown that preconditioning cells to lower oxygen level conditions can enable them to later withstand more severe hypoxia. Based on these observations, a team of scientists, led by Sang Hun Lee, hypothesized that preconditioning mesenchymal stem cells may help them survive and proliferate once they are transplanted into injured tissue.
To test their idea, the scientists preconditioned mesenchymal stem cells from people’s fat tissue to low oxygen levels and then transplanted the cells into mice whose blood supply had been cut off to certain tissues. When they compared the impact of transplanting these preconditioned cells to transplanting cells that were not preconditioned, they found that the preconditioned cells survived and proliferated at higher rates and that they were more effective in helping the mice recover functionally. These results add to the breadth of research that suggests that stem cells may have an array of therapeutic applications and that any limitations that arise may be able to be addressed by combining stem cell transplantation with other strategies.
Learn more about the benefits of stem cell therapy.
Reference
Zhao, Yan et al. (2016). Hypoxia-induced expression of cellular prion protein improves the therapeutic potential of mesenchymal stem cells. Cell Death and Disease, 7, e2395.

by admin | Jul 25, 2016 | Stem Cell Research, Studies
Research has pointed strongly toward autologous adipose tissue-derived mesencymal stem cells (AdMSC‘s) as a treatment option for a number of neurological diseases. There is growing evidence that these cells can successfully differentiate into neurons in the brain, thereby protecting the brain against certain diseases of the central nervous system. Adipose tissue is particularly attractive when seeking to use mesenchymal stem cells (MSC’s) because it is easy to retrieve MSCs in this type of tissue. Now, a case study published in the Journal of Medical Case Reports demonstrates how AdMSC‘s were successfully used to treat a patient suffering from progressive supranuclear palsy (PSP), a disorder closely related to Parkinson’s disease.
There are currently no good treatment options for PSP. Dopaminergic drugs that are used for Parkinson’s disease are often implemented with PSP patients because of clinical similarities in these diseases. However, the benefits are both minor and short-lived. As described in this case report, researchers successfully used a novel form of therapy on a 71-year old South Korean man with PSP.
The man was examined before his treatment and continually for six months afterwards. The AdMSC protocol improved the patient’s performance on the Progressive Supranuclear Palsy Rating Scale (PSPRS) and improved both his cognitive performance and his ability to conduct daily activities. In addition to the treatment’s efficacy, it also bore limited safety concerns, as mild fever and short-term elevated blood pressure were the only adverse side affects observed with the procedure.
The patient underwent four intrathecal and five intravenous infusions infusions of AdMSC’s to increase the chances of clinical efficacy. Specifically, the strategy of the intrathecal infusions was to increase the likelihood of getting the AdMSC’s into the central nervous system. However, because the intrathecal cavity is narrow, the dosage that can be achieved through this route is limited. Thus, intravenous injections were administered as a way to increase the dosage amount. Though this success of AdMSC’s administration in PSP is just the beginning, it represents great potential for the use of stem cells in this rare but deadly disorder.
To learn more about the safety of adipose stem cell procedure, click here.
Reference
Choi, S.W., Park, K.B., Woo, S.K., Kang, S.K., & Ra, J.C. (2014). Treatment of progressive supranuclear palsy with autologous adipose tissue-derived mesenchymal stem cells: a case report. Journal of Medical Case Reports, 8(87), 1-5.

by admin | Feb 29, 2016 | Stem Cell Research, Studies
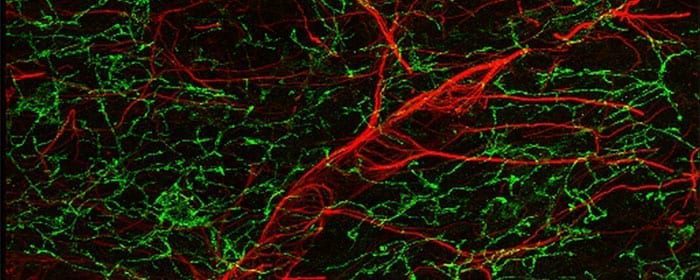
Scientists have identified a new way to treat disorders of the brain using stem cells. Their proposed technique is particularly promising because of the ability of stem cells to cross the blood brain barrier, a barrier that has posed challenges for other drug candidates.
A recent review published by Rutgers University’s Pranela Rameshwar and colleagues supports the notion that stem cells, and particularly, mesenchymal stem cells (or MSCs) may be great drug delivery vehicles for people with neurological diseases such as Alzheimer’s disease, Parkinson’s disease, traumatic brain injury, and certain forms of brain cancer. Therapies that are currently used suffer a number of limitations that could potentially be overcome by stem cell delivery of drugs.
Not only are several drug substances unable to cross the blood brain barrier, but drugs can also have unwanted toxic effects because it is difficult to specifically target their action to the areas where they are needed. Stem cells can help ensure that drugs are delivered specifically to the brain, and perhaps even to the specific parts of the brain where the drug could be helpful. The use of stem cells could also circumvent the need to perform highly invasive surgical procedures to address neurological diseases.
Though different types of stem cells could theoretically be used to deliver therapies to the brain, mesenchymal stem cells appear highly valuable because research has shown them to be safe. Unlike other forms of stem cells, MSCs do not tend to form tumors and also preferentially migrate to parts of the brain in need of new tissue. An additional advantage of MSCs is that their use is not subject to the same ethical scrutiny as some other stem cells. Now that the therapeutic potential for MSCs has been identified, relevant research efforts will undoubtedly increase, with the hopes of translating this promising therapeutic approach into practice.
Learn about the use of adipose stem cells to treat brain injury here.
Reference
Aleynik, A., Gernavage, K. M., Mourad, Y., Sherman, L. S., Liu, K., Gubenko, Y. A., & Rameshwar, P. (2014). Stem cell delivery of therapies for brain disorders. Clin Transl Med, 3, 24. doi: 10.1186/2001-1326-3-24






 St. Petersburg, Florida
St. Petersburg, Florida
