
by admin | Mar 22, 2018 | Parkinson's Disease, Stem Cell Research
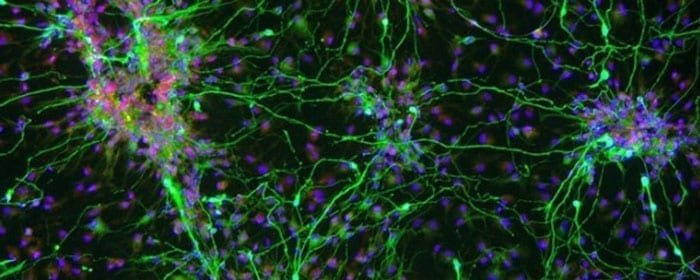
A recent review has outlined the potential of using stem cells to treat Parkinson’s Disease. Parkinson’s Disease patients have been limited by the realities of their treatment options. Generally, treatments act to relieve symptoms that occur with Parkinson’s Disease rather than the underlying cause. More specifically, by substituting a brain chemical called dopamine, or by trying to enhance the effects that naturally occurring dopamine has in the brain, these treatments aim to reduce the motor symptoms that are commonly associated with the disease. Unfortunately, none of these treatments can actually regenerate the dopamine neurons that are destroyed by the disease.
Given the potential for stem cells to replace critical cell groups, researchers in neuroscience have reasoned that stem cells could provide a cell-based therapy for Parkinson’s Disease patients. Given that a loss of dopaminergic functioning in a key feature of the disease, using stem cells to restore this functioning could potentially relieve symptoms and also slow the progression of the disease.
Based on this rationale, researchers have wanted to perform clinical trials to determine how stem cells impact Parkinson’s Disease patients. Based on the research thus far, it seems that mesenchymal stem cells are the best candidate for cell-based therapies against Parkinson’s disease. However, there are several details that need to be worked out to determine which tissue or tissues would be best for deriving these stem cells and exactly how to use the stem cells to help patients. For instance, according to the authors of the review, it is likely that Parkinson’s Disease patients will need the transplant of cells that produce another brain chemical, serotonin, in addition to those that produce dopamine because serotonin is implicated in the non-motor symptoms of the disease.
Research to develop cell-based therapies for Parkinson’s Disease is still in its infancy. However, as our understanding of the disease itself – as well as of how stem cells can be used to treat neurodegenerative diseases – we will hopefully start to leverage stem cells to develop effective therapies that help Parkinson’s Disease patients.
Learn more about our stem cell treatment for Parkinson’s Disease here.

by admin | Mar 20, 2018 | Heart Failure, Stem Cell Research
A recent study, published in Circulation Research, has shown how umbilical cord mesenchymal stem cells may help patients who suffer from heart failure. The researchers observed patients with heart failure that was chronic and stable and that presented with reduced ejection fraction. Ejection fraction refers to the percentage of blood that leaves the heart each time the heart contracts and is normally 55% or higher. A reduced ejection fraction can indicate weakness, damage, or other problems.
In their investigation, the scientists aimed to evaluate whether infusing umbilical cord mesenchymal stem cells in this group of heart failure patients is safe – and whether the cells could improve any of the clinical features of heart failure in these patients. To do this, they infused 15 patients with umbilical cord mesenchymal stem cells and used a placebo in 15 other patients. They then tested patients for adverse side effects on the day they underwent infusions, as well as 15 and 90 days after the procedure.
None of the patients who underwent mesenchymal stem cell infusions exhibited adverse side effects over the period of time in which they were observed. Additionally, none of the patients tested positive for antibodies against the stem cells, meaning that the patients’ immune systems were not negatively reacting to the infusions. Based on these results, the researchers concluded that the mesenchymal stem cell transplants were safe for this group of heart failure patients.
The researchers also tested the patients’ cardiac function and quality of life 3, 6, and 12 months after the mesenchymal stem cell infusions. To do so, the scientists used imaging to look at the heart, employed ejection fraction level tests, and implemented what are known as the New York Heart Association functional class and Minnesota Living with Heart Failure Questionnaire.
The scientists’ tests showed that ejection fraction increased in the patients who had undergone mesenchymal stem cell infusions, with the most significant increase apparent at 6-month post-infusion. The patients who had received the placebo treatment, on the other hand, did not show any change in ejection fraction. Functional status and quality of life were also better because of mesenchymal stem cell infusion than placebo. Future studies will help us better understand how we can use these cells to help those with heart failure.
Learn about the regenerative potential of Mesenchymal stem cells here.

by admin | Mar 17, 2018 | Stem Cell Research
Degenerative joint diseases like Osteoarthritis are difficult to effectively treat, as total joint arthroplasties are often associated with poor outcomes. Following these surgeries, many patients need additional interventions. As such, clinicians and researchers have begun to turn to new therapeutic options for degenerative joint diseases. Stem cells offer one promising route for these types of therapies, and clinical data have shown that patients with knee osteoarthritis have experienced less pain after stem cell transplants. A recent article, published in Arthroscopy Techniques, lays out a way to use stem cell transplantation to help patients with degenerative joint disease of the knee.
Mesenchymal stem cells are good candidates for helping with degenerative disease because of their ability to differentiate into chondrocytes, the cells that make up joints. In many cases, therapies are formed based on the use of mesenchymal stem cells that come from either fat tissue (called adipose tissue) or bone marrow tissue. In the current article, the authors lay out the process for using adipose-derived stem cells for degenerative joint disease of the knee. The authors focus on this type of stem cell because adipose tissue has been shown to be richer in mesenchymal stem cells and are less likely to lead to certain types of complications. For instance, they have been shown to have an anti-inflammatory response that helps to modify immune activity.
In this technique, the stem cells themselves are extracted from adipose tissue using liposuction, which is minimally invasive. The authors also detail how to position the patient for the stem cell extraction procedure in order to achieve optimal results. They explain exactly how to extract the cells and then how to process them. Finally, they detail how to go about injecting the stem cells into the patient with neurodegenerative joint disease of the knee and what is needed for the patient postoperatively.
The use of adipose-derived stem cell transplants for degenerative joint disease is still relatively new. However, that researchers are putting focused efforts and resources into developing detailed best practices for these types of interventions suggests that these types of therapies will be used more in the future and that the procedures will improve over time as we collect more relevant data.
Learn about our stem cell therapy for Osteoarthritis here.

by admin | Mar 16, 2018 | Stem Cell Research
With the growing realization that stem cells can help countless patients suffering from various diseases and injuries has come more research into how stem cells can best be used for these purposes. The questions not only involve which patients can benefit and how, but also which types of stem cells are useful and for what purposes, and how each beneficial stem cell type can be best incorporated into different therapeutic approaches. A new publication in Stem Cells and Development covers the specific advantages of stem cells that are derived from human Wharton’s jelly, which comes from the umbilical cord.
Mesenchymal stem cells are often used for clinical purposes, and the gold standard tissue for isolating mesenchymal stem cells has been bone marrow tissue. A distinct advantage of human Wharton’s jelly-derived stem cells over bone marrow-derived stem cells is the ease with which they are isolated. Not only is it technically relatively simple to retrieve stem cells from the umbilical cord, but it is less invasive than doing so from the bone marrow.
In the current study, the researchers characterized the best way to isolate the mesenchymal stem cells from the Wharton’s jelly and also compared the stem cells that come from Wharton’s jelly to those that come from the bone marrow. According to their analysis, some of the critical advantages of mesenchymal stem cells deriving from Wharton’s jelly rather than from bone marrow are the relative abundance of genes associated with immune system functioning, cell adhesion, and proliferation. Each of these functions is important for stem cell therapeutic applications, and so having more genes that support these functions s beneficial.
The researchers also observed specific ways in which Wharton’s jelly mesenchymal stem cells affect the immune system. Based on their observations, they concluded that these stem cells are attractive candidates for therapies that target diseases of the central nervous system, including Parkinson’s disease, multiple sclerosis, and amyotrophoic lateral sclerosis (also known as ALS). Further research will help to clarify the potential of Wharton’s jelly, and more comparative research like that performed in this study will help us understand the best ways to use different stem cells for different therapeutic functions.

by admin | Mar 14, 2018 | Heart Failure, Stem Cell Research
Heart failure is currently treated using pharmacologic interventions that help to control the symptoms of heart failure and slow the process of deterioration. However, these drugs do not stop problematic processes occurring at the cellular level, and so patients using these drugs continue to decline toward end-stage heart failure. Because the progression of heart failure involves things like cardiac remodeling and fibrosis at the cellular level, researchers have reasoned that cell-based therapies may be a promising way to treat heart failure patients. A recent review published in Stem Cells International outlines the rationale for using mesenchymal stem cells to treat heart failure and presents data from relevant clinical trials.
Mesenchymal stem cells are an attractive type of stem cell for both research clinical applications because of their ease of accessibility. These cells can be retrieved from a number of tissues, including fat tissue, heart tissue, umbilical cord tissue, and bone marrow tissue. A number of properties of mesenchymal stem cells also make them a promising therapeutic option for heart failure and other diseases. For instance, they have been shown to reduce inflammation and the initiation of inflammation and to promote the growth of blood vessels. Indeed, it has been suggested that the central process of heart failure is inflammation.
In cardiology, many of the clinical trials that have been performed with mesenchymal stem cells have focused on ischemic heart failure, though there are data demonstrating the promise of these stem cells in both ischemic and non-ischemic heart failure. While there are not as many data on the impact of mesenchymal stem cells on non-ischemic heart failure patients, the authors of the review argue that these cells could be even more advantageous in this group of patients (versus those with ischemic heart failure) because the damaged part of the heart still has adequate blood supply in the case of non-ischemic heart failure.
Overall, studies have tended to show that mesenchymal stem cells are a safe option, with little risk for significant adverse side effects. Clinical trials have helped to elucidate the specific ways that mesenchymal stem cells can be used to help with heart failure. Cellular scaffolds, for example, can be used to ensure that the stem cells are able to reach the target area of the heart in enough abundance to have an impact. Future studies will help to clarify the contexts in which these cells can be useful – and how their use can be optimized to help patients.

by admin | Feb 16, 2018 | Stem Cell Research
A popular type of stem cell in the research and clinical communities is what is known as the adipose tissue-derived mesenchymal stem cell, which are stem cells that come from fat tissue. A review published last year in Stem Cells International has provided a comprehensive picture of what makes these stem cells beneficial for treating disease and injury.
One characteristic of adipose tissue-derived mesenchymal stem cells that originally made them popular is the ease with which they are accessed. Gaining access to fat tissue is relatively simple compared to accessing other types, such as those from the bone marrow. Other attractive features have been their abundance and the ability to use them with no ethical concerns.
While all adipose tissue-derived mesenchymal stem cells have these advantageous features, there are a number of types of adipose tissue-derived mesenchymal stem cells, and researchers are still working to determine the relative advantages of each of these types. For instance, there are types that come from white adipose tissue and types that come from brown adipose tissue. Much brown adipose tissue exists in fetuses and newborns and transforms to white adipose tissue with aging. Understanding how these different types of adipose tissue work therapeutically will be important for determining when and how to use these cell types. Overall, though, it seems that adipose tissue-derived mesenchymal stem cells from younger patients proliferate at higher rates than those from older patients.
Adipose tissue-derived mesenchymal stem cells also differ in their properties depending on how they were harvested and the environment in which they are put. The two procedures for harvesting these cells are called resection and lipoaspiration. One study found that when cells were extracted with lipoaspiration, a higher abundance of cells could be obtained, whereas the proliferation of the cells was similar with both harvesting procedures. Environmental factors, including which trophic factors are present, the hydrostatic pressure, and the fluid sheer stress, also impact the ability of the cells to proliferate and differentiate. Other factors, such as the specific growth factors produced and the surface markers that are present, also impact the utility of adipose tissue-derived mesenchymal stem cells.





 St. Petersburg, Florida
St. Petersburg, Florida
