
by admin | Apr 19, 2018 | Multiple Sclerosis, Stem Cell Research
Multiple sclerosis is a neurodegenerative disease that occurs when the immune system attacks the material that insulates nerve cells. As the immune system breaks down these myelin sheaths that coat the nerves, it becomes progressively more difficult for cells of the nervous system to communicate with one another. A new study on the potential use of stem cells to treat multiple sclerosis has led to promising results.
Because stem cells – and specifically, mesenchymal stem cells have been used to treat other immune conditions and inflammatory conditions successfully, scientists have reasoned that these stem cells may be able to help with multiple sclerosis. In this recent study, published in the Journal of Translational Medicine this year, scientists aimed to determine if umbilical cord mesenchymal stem cells are safe in patients with multiple sclerosis and if they may have any impact on the disease.
The study involved a full year investigation into 20 participants who had multiple sclerosis. The mean age for enrollees was approximately 41 years, and 60% of participants were female. One-quarter of the subjects did not take any medications for their multiple sclerosis over the course of the study. All subjects received seven infusions of stem cells over the course of one week. Their neurological and imaging tests to assess subjects’ neurological status were implemented before the infusions, as well as one month after and one year after the treatment.
The researchers determined that the stem cell regimen was safe, as no patients suffered any serious adverse side effects during the course of treatment. There were some complaints of headaches and fatigue, however. The researchers also concluded that the stem cell therapy was effective in helping the multiple sclerosis patients, as several of their scores improved one month after the treatment. In addition to performance measures, reported quality of life also improved with the treatment. Impressively, inactive lesions were observed in the majority of MRI scans of the brain and spinal cord (83.3%) one year after treatment.
Twenty percent of the participants reduced their medication in the follow-up period. These promising results suggest that stem cells may be able to help multiple sclerosis patients and that these types of treatments need to be further explored for their potential to help this set of patients.

by admin | Apr 4, 2018 | Stem Cell Research
Diabetic foot ulcer, which, by 2030, is projected to occur in 25% of patients who suffer from diabetes, does not currently have an attractive treatment option. The therapies that are used today are expensive, require long-term stays in the hospital, and are often not associated with complete recovery. As such, cell-based therapies have been under investigation for their potential to help with the development of an effective therapeutic approach for diabetic foot ulcer. A recent case report describes the use of placenta-derived mesenchymal stem-cell hydrogel in a patient with diabetic foot ulcer and demonstrates the potential promise of this strategy.
The patient covered in this case report is a 57-year old female who has type 2 diabetes and had suffered from diabetic foot ulcer on her right foot for 20 days. Conventional therapies had made no impact on the foot ulcer. Following conventional approaches, the patient received stem-cell hydrogel topical wound treatment, where the clinicians filled the entire wound surface with gel and observed and cleaned the wound daily for 3 weeks.
The ulcer significantly improved with the use of the hydrogel treatment. Not only did the wound almost fully heel, but the patient’s foot function was also well preserved. The patient was able to walk normally. The treatment was not associated with any complications, and there was no recurrence of the ulcer during the 6-month follow-up period.
Based on their observations of the effect of the placenta-derived mesenchymal stem cell hydrogel on a patient’s diabetic foot ulcer, the authors of this case study concluded that the hydrogel may be an effective strategy for the treatment of diabetic foot ulcer. According to the authors, this was the first patient in the world to receive this hydrogel treatment for diabetic foot ulcer. Thus, the results set the stage for more research into how this hydrogel and other stem cell treatments may be used to help with diabetes complications such as diabetic foot ulcer.

by admin | Apr 2, 2018 | Stem Cell Research
A recent publication in Advanced Experimental Medicine and Biology has pointed to the ways that stem cell technology is not only helping us to develop promising therapeutics for a number of diseases, but it is also helping us advance our understanding of a number of brain disorders.
The authors point to well-known diseases like Parkinson’s Disease and Alzheimer’s Disease – that, despite much attention, funding, and research, are still not preventable or fully curable diseases. They also point to less well-known diseases like fragile X syndrome, Angelman syndrome, Prader-Willi syndrome, and Rett syndrome.
Fragile X syndrome affects more males than females and delayed speech and language development. It is characterized by learning disabilities and deficits in cognition.
Similarly, Angelman syndrome, which is rare, is associated with developmental delays. However, those affected by this syndrome also suffer from balance disturbances, seizures, and difficulties with walking.
Prader-Willi syndrome leads to weak muscle tone and affects many parts of the body. Physical development is therefore what tends to be delayed in this syndrome. Type 2 Diabetes and obesity are common complications.
Patients with Rett syndrome are almost always female and display repetitive hand motions constantly while they are awake. These patients experience difficulties across a spectrum of functions, including speaking, eating, walking, and breathing.
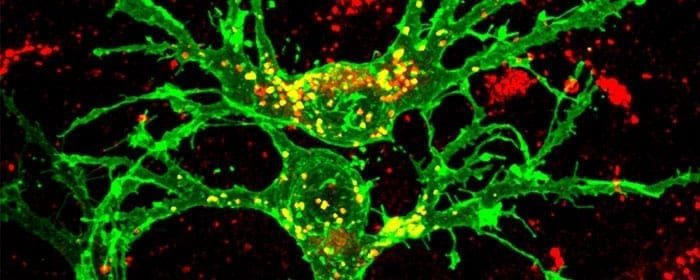
All these diseases that authors of this publication discuss have genetic underpinnings, and, according to the authors, can be investigated in new ways thanks to stem cell technologies. What stem cell technology affords is an enormous source of brain cells and their precursors that can be used to help model these diseases and to observe how different factors affect aspects of the disease.
With better models, tests of therapeutics become more robust as well. The hope is that eventually, stem cells will enable us to understand (epi)genetic brain disorders and also develop ways to effectively prevent or treat them.

by admin | Mar 28, 2018 | Parkinson's Disease, Stem Cell Research
Recently, researchers transplanted stem cells into patients suffering from Parkinson’s Disease and observed promising results, particularly with respect to the safety of using stem cells in this group of patients. The specific type of stem cells used are called autologous bone-marrow-derived mesenchymal stem cells. These cells have been deemed promising candidates for treating Parkinson’s patients for a variety of reasons, and so researchers have begun to use them in patients. The hope is that as we collect more and more data, we will gain a more comprehensive understanding of if and how these cells can improve the lives of those with Parkinson’s Disease.
In the current study, researchers transplanted the bone-marrow-derived mesenchymal stem cells in 7 patients with Parkinson’s Disease. The patients ranged in age from 22 to 62. The patients were then followed for a period of 10 to 36 months. The researchers used measures such as the Unified Parkinson’s Disease Rating Scale (UPDRS), the Hoen and Yahr (H&Y), and Schwab and England (S&E) scores to evaluate Parkinsonian symptoms in these patients.
Given that the researchers did not observe any major adverse side effects, they conclude that the use of these stem cells in Parkinson’s Disease patients appears to be safe. They also found it promising that certain Parkinson’s Disease symptoms improved in some patients following stem cell transplantation. For instance, facial expression, freezing episodes, and patients’ gaits showed some improvement. However, given that these observations were subjective, the researchers are careful to mention that they cannot claim that the stem cells caused the improvements that were observed. Nonetheless, 2 of the patients were able to significantly reduce their doses of their Parkinson’s medications.
This study was uncontrolled and involved a small number of patients, so future research is needed to better understand the potential of bone-marrow-derived mesenchymal stem cells for helping Parkinson’s Disease patients. However, it is promising to see that there were no adverse side effects in this group of patients and that some symptoms appeared to improve.

by admin | Mar 26, 2018 | Stem Cell Research
Therapies using stem cells are becoming more and more popular over time, and research is helping to clarify how these types of therapies can help patients. A new review published this year in the Journal of Cosmetic and Laser Therapy has provided a comprehensive description of the ways stem cells may be used for plastic and cosmetic surgeries.
Though many different stem cell types have been investigated for their potential to help achieve desired aesthetic results through plastic and cosmetic surgeries, adipose-derived mesenchymal stem cells appear to be the most promising, based on current research. These types of stem cells are known to produce proteins that become deficient during aging and that are characteristic of youthful, undamaged skin.
Studies have shown that adipose-derived mesenchymal stem cells can improve the thickness of the skin and increase cellular proliferation and differentiation. These features are not only beneficial for helping with voluntary cosmetic procedures but can also help with wound healing, scar remodeling, fat grafting, and local tissue ischemia.
Adipose tissue offers advantages over other tissues that can provide stem cells, such as bone marrow. For instance, it is easier to retrieve stem cells from adipose tissue than from many other tissues. The cells from adipose tissue also tend not to have to be expanded within a lab, so they can often be used at the same time that they are extracted. This feature of adipose-derived mesenchymal stem cells makes them convenient to use and can reduce the pain and recovery time patients must endure when undergoing cell-based therapies.
Over time, researchers are likely to recognize the relative advantages of different types of stem cells for cosmetic and plastic surgery purposes. However, at this point, adipose-derived mesenchymal stem cells appear to provide the greatest opportunity to improve outcomes in these types of procedures.
Find out why Mesenchymal stem cells have regenerative potential by clicking here.

by admin | Mar 24, 2018 | Age Management, Stem Cell Research
Given the promising results that stem cells have shown for therapies against brain disease and disorders, researchers have reasoned that stem cells could also be useful for age-related neurodegenerative disease and stroke. Aging indeed is related to several of the physiological changes that occur in the brains of those who suffer from neurodegenerative disorders. A recent review published in Ageing Research and Reviews outlines the ways stem cells may be used for cell-based therapies in stroke and neurodegeneration, as well as the benefits and limitations of stem cell approaches to these pathological conditions.
According to the authors, stem cells can be used to help with a number of the physiological marks of neurodegeneration. Loss of neurons and synapses is one of the more direct ways that stem cells can potentially help. By replacing these neural elements, stem cells can potentially reverse the impact of their loss. These functions may include both motor and cognitive aspects.
In addition to the loss of cell bodies and neural gray matter, the white matter of the brain is also affected by aging. The axons that connect cells to one another lose their plasticity and ability to repair themselves over time. These types of dysfunctions represent other ways that stem cells may be able to help with age-related neurodegenerative disorders.
Other problematic aspects of aging and associated neuropathologies are oxidative stress and misfolded proteins. While there has been some research to suggest that stem cells may be relevant for these issues, more research is needed to understand how stem cells may be able to help with neurodegeneration that results from these features that are often associated with aging. While the role of stem cells may be clearer when it comes to other aspects of neurodegeneration, future research will also help us understand how we can best apply this knowledge to help those suffering from neurodegenerative disease – age-related and otherwise.
Learn more about our stem cell therapy for age management here.





 St. Petersburg, Florida
St. Petersburg, Florida
