
by admin | Apr 19, 2018 | Multiple Sclerosis, Stem Cell Research
Multiple sclerosis is a neurodegenerative disease that occurs when the immune system attacks the material that insulates nerve cells. As the immune system breaks down these myelin sheaths that coat the nerves, it becomes progressively more difficult for cells of the nervous system to communicate with one another. A new study on the potential use of stem cells to treat multiple sclerosis has led to promising results.
Because stem cells – and specifically, mesenchymal stem cells have been used to treat other immune conditions and inflammatory conditions successfully, scientists have reasoned that these stem cells may be able to help with multiple sclerosis. In this recent study, published in the Journal of Translational Medicine this year, scientists aimed to determine if umbilical cord mesenchymal stem cells are safe in patients with multiple sclerosis and if they may have any impact on the disease.
The study involved a full year investigation into 20 participants who had multiple sclerosis. The mean age for enrollees was approximately 41 years, and 60% of participants were female. One-quarter of the subjects did not take any medications for their multiple sclerosis over the course of the study. All subjects received seven infusions of stem cells over the course of one week. Their neurological and imaging tests to assess subjects’ neurological status were implemented before the infusions, as well as one month after and one year after the treatment.
The researchers determined that the stem cell regimen was safe, as no patients suffered any serious adverse side effects during the course of treatment. There were some complaints of headaches and fatigue, however. The researchers also concluded that the stem cell therapy was effective in helping the multiple sclerosis patients, as several of their scores improved one month after the treatment. In addition to performance measures, reported quality of life also improved with the treatment. Impressively, inactive lesions were observed in the majority of MRI scans of the brain and spinal cord (83.3%) one year after treatment.
Twenty percent of the participants reduced their medication in the follow-up period. These promising results suggest that stem cells may be able to help multiple sclerosis patients and that these types of treatments need to be further explored for their potential to help this set of patients.

by admin | Apr 4, 2018 | Stem Cell Research
Diabetic foot ulcer, which, by 2030, is projected to occur in 25% of patients who suffer from diabetes, does not currently have an attractive treatment option. The therapies that are used today are expensive, require long-term stays in the hospital, and are often not associated with complete recovery. As such, cell-based therapies have been under investigation for their potential to help with the development of an effective therapeutic approach for diabetic foot ulcer. A recent case report describes the use of placenta-derived mesenchymal stem-cell hydrogel in a patient with diabetic foot ulcer and demonstrates the potential promise of this strategy.
The patient covered in this case report is a 57-year old female who has type 2 diabetes and had suffered from diabetic foot ulcer on her right foot for 20 days. Conventional therapies had made no impact on the foot ulcer. Following conventional approaches, the patient received stem-cell hydrogel topical wound treatment, where the clinicians filled the entire wound surface with gel and observed and cleaned the wound daily for 3 weeks.
The ulcer significantly improved with the use of the hydrogel treatment. Not only did the wound almost fully heel, but the patient’s foot function was also well preserved. The patient was able to walk normally. The treatment was not associated with any complications, and there was no recurrence of the ulcer during the 6-month follow-up period.
Based on their observations of the effect of the placenta-derived mesenchymal stem cell hydrogel on a patient’s diabetic foot ulcer, the authors of this case study concluded that the hydrogel may be an effective strategy for the treatment of diabetic foot ulcer. According to the authors, this was the first patient in the world to receive this hydrogel treatment for diabetic foot ulcer. Thus, the results set the stage for more research into how this hydrogel and other stem cell treatments may be used to help with diabetes complications such as diabetic foot ulcer.

by admin | Mar 28, 2018 | Parkinson's Disease, Stem Cell Research
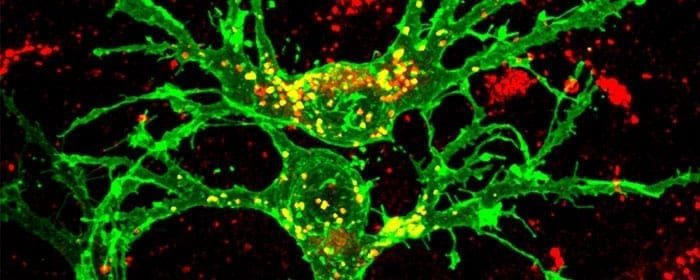
Recently, researchers transplanted stem cells into patients suffering from Parkinson’s Disease and observed promising results, particularly with respect to the safety of using stem cells in this group of patients. The specific type of stem cells used are called autologous bone-marrow-derived mesenchymal stem cells. These cells have been deemed promising candidates for treating Parkinson’s patients for a variety of reasons, and so researchers have begun to use them in patients. The hope is that as we collect more and more data, we will gain a more comprehensive understanding of if and how these cells can improve the lives of those with Parkinson’s Disease.
In the current study, researchers transplanted the bone-marrow-derived mesenchymal stem cells in 7 patients with Parkinson’s Disease. The patients ranged in age from 22 to 62. The patients were then followed for a period of 10 to 36 months. The researchers used measures such as the Unified Parkinson’s Disease Rating Scale (UPDRS), the Hoen and Yahr (H&Y), and Schwab and England (S&E) scores to evaluate Parkinsonian symptoms in these patients.
Given that the researchers did not observe any major adverse side effects, they conclude that the use of these stem cells in Parkinson’s Disease patients appears to be safe. They also found it promising that certain Parkinson’s Disease symptoms improved in some patients following stem cell transplantation. For instance, facial expression, freezing episodes, and patients’ gaits showed some improvement. However, given that these observations were subjective, the researchers are careful to mention that they cannot claim that the stem cells caused the improvements that were observed. Nonetheless, 2 of the patients were able to significantly reduce their doses of their Parkinson’s medications.
This study was uncontrolled and involved a small number of patients, so future research is needed to better understand the potential of bone-marrow-derived mesenchymal stem cells for helping Parkinson’s Disease patients. However, it is promising to see that there were no adverse side effects in this group of patients and that some symptoms appeared to improve.

by admin | Mar 22, 2018 | Parkinson's Disease, Stem Cell Research
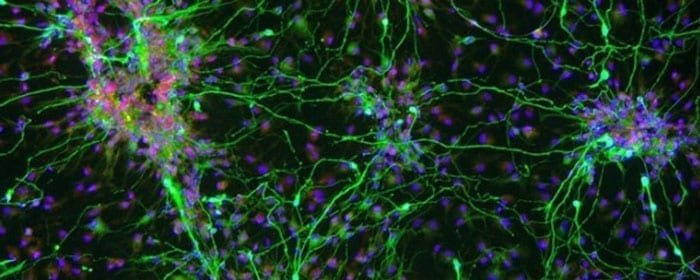
A recent review has outlined the potential of using stem cells to treat Parkinson’s Disease. Parkinson’s Disease patients have been limited by the realities of their treatment options. Generally, treatments act to relieve symptoms that occur with Parkinson’s Disease rather than the underlying cause. More specifically, by substituting a brain chemical called dopamine, or by trying to enhance the effects that naturally occurring dopamine has in the brain, these treatments aim to reduce the motor symptoms that are commonly associated with the disease. Unfortunately, none of these treatments can actually regenerate the dopamine neurons that are destroyed by the disease.
Given the potential for stem cells to replace critical cell groups, researchers in neuroscience have reasoned that stem cells could provide a cell-based therapy for Parkinson’s Disease patients. Given that a loss of dopaminergic functioning in a key feature of the disease, using stem cells to restore this functioning could potentially relieve symptoms and also slow the progression of the disease.
Based on this rationale, researchers have wanted to perform clinical trials to determine how stem cells impact Parkinson’s Disease patients. Based on the research thus far, it seems that mesenchymal stem cells are the best candidate for cell-based therapies against Parkinson’s disease. However, there are several details that need to be worked out to determine which tissue or tissues would be best for deriving these stem cells and exactly how to use the stem cells to help patients. For instance, according to the authors of the review, it is likely that Parkinson’s Disease patients will need the transplant of cells that produce another brain chemical, serotonin, in addition to those that produce dopamine because serotonin is implicated in the non-motor symptoms of the disease.
Research to develop cell-based therapies for Parkinson’s Disease is still in its infancy. However, as our understanding of the disease itself – as well as of how stem cells can be used to treat neurodegenerative diseases – we will hopefully start to leverage stem cells to develop effective therapies that help Parkinson’s Disease patients.
Learn more about our stem cell treatment for Parkinson’s Disease here.

by admin | Mar 17, 2018 | Stem Cell Research
Degenerative joint diseases like Osteoarthritis are difficult to effectively treat, as total joint arthroplasties are often associated with poor outcomes. Following these surgeries, many patients need additional interventions. As such, clinicians and researchers have begun to turn to new therapeutic options for degenerative joint diseases. Stem cells offer one promising route for these types of therapies, and clinical data have shown that patients with knee osteoarthritis have experienced less pain after stem cell transplants. A recent article, published in Arthroscopy Techniques, lays out a way to use stem cell transplantation to help patients with degenerative joint disease of the knee.
Mesenchymal stem cells are good candidates for helping with degenerative disease because of their ability to differentiate into chondrocytes, the cells that make up joints. In many cases, therapies are formed based on the use of mesenchymal stem cells that come from either fat tissue (called adipose tissue) or bone marrow tissue. In the current article, the authors lay out the process for using adipose-derived stem cells for degenerative joint disease of the knee. The authors focus on this type of stem cell because adipose tissue has been shown to be richer in mesenchymal stem cells and are less likely to lead to certain types of complications. For instance, they have been shown to have an anti-inflammatory response that helps to modify immune activity.
In this technique, the stem cells themselves are extracted from adipose tissue using liposuction, which is minimally invasive. The authors also detail how to position the patient for the stem cell extraction procedure in order to achieve optimal results. They explain exactly how to extract the cells and then how to process them. Finally, they detail how to go about injecting the stem cells into the patient with neurodegenerative joint disease of the knee and what is needed for the patient postoperatively.
The use of adipose-derived stem cell transplants for degenerative joint disease is still relatively new. However, that researchers are putting focused efforts and resources into developing detailed best practices for these types of interventions suggests that these types of therapies will be used more in the future and that the procedures will improve over time as we collect more relevant data.
Learn about our stem cell therapy for Osteoarthritis here.




 St. Petersburg, Florida
St. Petersburg, Florida
