
by admin | Jul 20, 2018 | Stem Cell Research, Stem Cell Therapy
Adipose treatment is a procedure in which stem cells are derived from a section of the abdomen then used for therapeutic purposes. Adipose-derived stem cells (ADSCs) are less invasive to extract compared to cells derived from other sources, such as bone marrow. In therapeutic applications, adding platelet-rich plasma (PRP) to ADSCs has been shown to have benefits.
What is PRP?
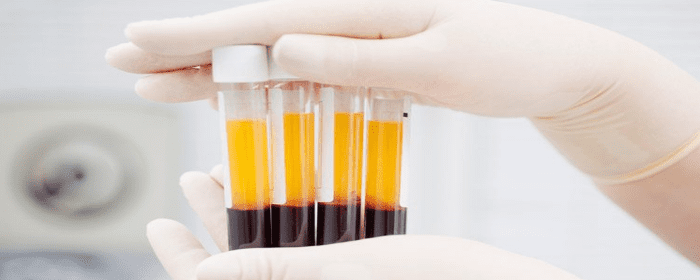
PRP therapy is the process by which a small sample of blood is removed from the patient. The platelets are then separated from other components of the blood via a centrifuge. The isolated platelets are shown to have high levels of diverse growth factors.
Why Are Growth Factors Important?
ADSCs are shown to have reduced proliferative potential. While they do secrete a wide range of growth factors, PRP therapy is coupled with stem cell therapy to maximize their regenerative medicine potential benefits by helping to increase their proliferation and differentiation. PRP essentially empowers the ADSCs, stimulating cell proliferation and cell differentiation when used for regenerative applications.
Which Applications Can the Therapy Be Used for?
Researchers have stated that the therapeutic potential of ADSCs is “enormous,” but by kickstarting the stem cells with PRP, it’s possible that the therapy will unlock even further medicinal possibilities. Anti-inflammatory and anti-apoptotic effects have been demonstrated by ADSCs, and there are many clinical trials which have either been completed or are ongoing to explore the treatment’s effects. Skeletal repair, soft tissue generation, and immune disorders such as Crohn’s disease and multiple sclerosis are just some of the therapeutic targets for this treatment. In specific, using ADSCs with PRP has been shown to aid periodontal tissue engineering, tendon repair, wound healing, and even bone regrowth.
Because the ADSCs are fairly easy to source and blood samples required for PRP are also simple to acquire, combining PRP to adipose stem cell therapy shows promise for delivering a powerful treatment that can address a broad variety of conditions, all with a minimally invasive approach.

by admin | Jul 19, 2018 | Stem Cell Research, Stem Cell Therapy, Studies
Under normal circumstances, pain receptors react to painful stimuli such as burns or lacerations. Pain receptors from the body then send that information along nerves to the brain via electrical signals. Once that electrical information reaches the brain (which happens almost immediately), it is perceived as pain. This type of pain is a nociceptive pain.
Neuropathic pain, however, is different. Neuropathic pain is caused by a condition of the nerves themselves. Patients with neuropathic pain experience chronic pain without any specific injury. Neuropathic pain may be felt as a burning sensation, tingling, or a “pins and needles” sensation, or these combined. Neuropathic pain most often occurs in people with diabetes, certain vitamin deficiencies, and shingles. It may also occur after people receive certain cancer treatments following a stroke.
While it is rather simple to treat pain caused by a burn or laceration (nociceptive pain), it is very difficult to effectively treat neuropathic pain. Standard treatments for neuropathic pain include anti-epilepsy medications such as phenytoin, gabapentin, or carbamazepine and antidepressants such as venlafaxine, duloxetine, or amitriptyline. Usually, these treatments are only modestly effective. Eventually, many patients need powerful opioid medications like morphine and oxycodone to control their pain.
Researchers at the Cleveland Clinic published research that strongly suggests that stem cells may be able to improve those battling neuropathic pain. Dr. Jianguo Cheng and his research group have shown that mesenchymal stem cell transplantation into the spinal fluid can reduce pain and pain sensitivity in an animal model of neuropathic pain. In one series of experiments, they showed that mesenchymal stem cells could relieve pain in rats who had experimental nerve damage. Researchers confirmed the benefit of stem cells for neuropathic pain in several different sets of experiments. The results have been so encouraging that Dr. Cheng and the Cleveland Clinic have applied to patent the technology.
Dr. Cheng’s group also showed intravenously administered mesenchymal stem cells are just as effective as cells administered into the spinal fluid (intrathecally). This is good news for patients since it is less invasive to put stem cells into a vein than it is to infuse them into the cerebrospinal fluid. Amazingly, the research group showed that stem cells injected through either route (vein or spinal fluid) ended up finding their way to damaged nerves where they could provide maximum benefit.
While this work in animals must be performed in humans to confirm the results, this preclinical research establishes a strong foundation for those clinical studies. These results provide hope to those who struggle with daily neuropathic pain.

by admin | Jul 10, 2018 | Hyperbaric Oxygen Therapy, Stem Cell Research, Stem Cell Therapy, Traumatic Brain Injury
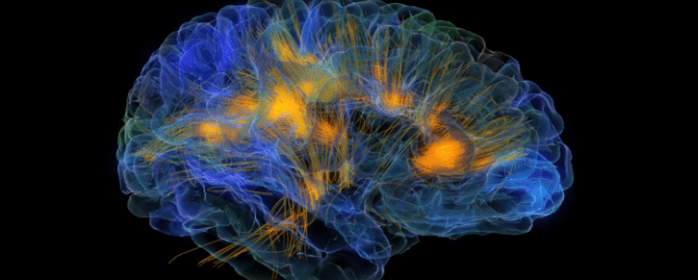
A technique called hyperbaric oxygen therapy (HBOT) has been shown to help patients with traumatic brain injury (TBI) who are suffering from a chronic neurological injury. HBOT appears to confer its benefits to these patients by increasing the neuroplasticity in the brain – or, in other words, by making it easier for the brain to re-wire itself. When the brain has a higher degree of neuroplasticity, it is easier to recover from neurological injuries because the brain can find ways to re-wire and restore functions that were lost due to damage to brain tissue.
A new study, published in Frontiers in Human Neuroscience, investigated the effects of HBOT on prolonged post-concussion syndrome (PPCS) that occurs as a result of TBI. The researchers used imaging strategies to monitor the brains of 15 patients with PPCS and evaluated the patients with tests of cognition. The researchers gave each patient 60 treatments with HBOT. The treatments were initiated anywhere from 6 months to 27 years after the patients had sustained their injuries.
Using imaging techniques called Dynamic Susceptibility Contrast-Enhanced and Diffusion Tensor Imaging (DTI) MR sequences, the researchers observed that HBOT increased blood flow and volume in the brain and that it led to the generation of new blood vessels. Using various cognitive tests, the researchers also found that HBOT improved memory, information processing speed, and executive functions.
Based on these findings, the researchers concluded that HBOT is beneficial for patients with TBI by inducing neuroplasticity in the brain, improving the integrity of microstructures of both white and gray matter within the brain, and allowing for the regeneration of nerve fibers. Future research will help clarify further benefits of HBOT and how the brain responds to this treatment.

by admin | Jul 9, 2018 | Health Awareness, Parkinson's Disease, Stem Cell Research, Studies
Parkinson’s disease is known to be a slowly progressing neurological disorder that can cause issues with the motor movement of the body. Signs of Parkinson’s disease can include severe stiffness, loss of balance, and lethargy. Although there are no cures for the condition, symptoms can be slowed down. However, most of the prescribed drugs for Parkinson’s disease can decrease in effectiveness over the course of time. This led to some investigation from researchers to consider the role of exercise as a treatment option. Initial studies revealed that exercise does reduce the symptoms and slowed the progression of the condition.
According to a recent phase 2 study, intense treadmill exercise can potentially reduce the progression symptoms of Parkinson’s disease. In this study, researchers treated exercise as a treatment and tracked the safety and effectiveness of different levels of exercise. The study consisted of 128 people that had been diagnosed with Parkinson’s disease and were not taking any medications nor exercised. The aerobic capacity, heartbeats and the severity of the disease were tested for a baseline.
The patients were divided into three groups. Group 1 was asked to continue living their life in a normal manner. Group 2 was asked to implement exercise in which they would walk on the treadmill daily for 30 minutes, four times a week. The speed of the treadmill was manipulated to maintain the heart rate of the participants between 60 to 65 percent of their maximum heart rate. Group 3 was asked to also implement exercise for the same amount of time but their heart rate was maintained in the range of 80 to 85 percent of their maximum rates. The patients were under supervision for the initial month and then asked to continue exercising on their own.
At the end of the six-month study, Group 1 showed their symptoms progressed further. Group 2 showed their symptoms progressed but not as much as Group 1. Group 3 showed almost no progression in their symptoms after following a heavier exercise regimen as the other groups. This study concluded that higher intensity exercise helped in decreasing the symptoms by improving the neuronal blood supply. Improved blood flow helps with the overall health of the brain and slows down the deterioration of the body.
The findings from the study are quite encouraging for patients who are recently diagnosed or early in their symptoms to have great benefits from the heavy exercise program. However, it is advised to consult with your physician prior to starting an exercise plan to avoid injuries and ensure your safety.

by admin | Jul 6, 2018 | Stem Cell Therapy, COPD, Stem Cell Research
Chronic obstructive pulmonary disease (COPD) is an incurable lung disorder which makes it difficult to breathe. It includes chronic bronchitis and emphysema and is characterized by a persistent cough and mucus production. While it is not curable, it can be managed through ongoing treatment to provide patients with effective symptom control and good quality of life. There are a few key types of lung damage that can occur in COPD:
- With emphysema, the air sacs (alveoli) in the lungs are compromised. The walls of alveoli are stretched and actually cause the lungs to expand, which makes it more difficult for air to move in and out.
- In chronic bronchitis, the bronchial tubes are constantly inflamed, which limits airflow. In specific, the cilia (hair-like structures in the airways) become damaged. The airway can also become swollen and clogged.
- Refractory asthma is also marked by swelling of the bronchial airways. Even medications cannot reverse the swelling.
Here, we examine a form of COPD treatment which has been gaining attention recently.
Blood-Derived PRP
Blood-derived platelet-rich plasma (PRP) therapy is increasingly being used to treat a broad range of conditions, including sports injuries and arthritis. The procedure is performed via intravenous blood extraction. After the blood cells are harvested, they are processed, and the platelets are separated from other blood components. With the higher concentration of platelets, the treated blood is then reinserted into the patient with the hopes of reducing inflammation and speeding up the body’s healing process.
The problem with blood-derived PRP is that the evidence illustrating the effectiveness of this treatment for COPD is lacking. While some studies have been performed and suggest the treatment’s ability to support hair regrowth and reduce osteoarthritis pain, the lack of definitive proof supporting PRP therapy’s ability to make a noticeable impact on COPD has spurred criticism.
A Better Alternative
Stem cell PRP takes PRP injections a step further by mixing platelets with stem cells to treat the structural airway issues present in all forms of COPD. In numerous studies, this approach has shown promise. Coupling blood derivatives with stem cell therapy have proven effective in tissue regeneration in areas like the knee and gums, for instance. In one report, researchers concluded that the therapy “offers a promising therapeutic approach that has shown potential in diverse degenerative lung diseases” based on findings across 15 separate studies.
Through traditional PRP treatment, platelets become 5-10 times more concentrated, or 150,000- 450,000 platelets per microliter. When combined with stem cells, however, they become supercharged and platelet counts are much higher. Because research suggests that the therapeutic level for platelet count should be closer to 1,000,000 per cubic milliliter, PRP and stem cells are far more powerful than PRP alone. Moreover, PRP therapy is derived from whole blood alone, meaning it contains very few CD34+ cells – the cells commonly found in the umbilical cord and bone marrow which have the greatest self-renewal capacity – if any.
With stem cell therapy for COPD, it is guaranteed that these cells will be introduced into the body in a higher concentration. They can then promote the healing process, replacing countless cells throughout the entire body, including the lung tissue.

by admin | Jul 2, 2018 | Stem Cell Research
There is a common misconception in the world of regenerative medicine that a patient may reach an age at which stem cell treatment will no longer be effective. In fact, the conditions which respond best to stem cell treatments are most common in elderly populations. Degenerative joint disorders, for instance, are ideal for stem cell therapy. Yet, they are often addressed instead with ineffective treatments such as over-the-counter painkillers or invasive procedures including total knee replacements.
The problem lies in the fact that elderly patients face greater risks for challenges following knee and hip reconstructions or replacements than younger individuals, including increased lengths of hospital stays and postoperative complications. But are elderly patients also more inclined to experience barriers with stem cell treatment? The answer is no – as long as the proper approach is used.
Types of Stem Cells
There are a few different ways stem cells can be used for therapy. Stem cells may be taken from a patient’s own bone marrow or fat deposits (called adipose stem cell therapy); or, they can be harvested from umbilical cord tissues. The latter is the second-youngest stem cells, outside of embryonic stem cells. Thus, they are considered the purest and most capable of functioning effectively and quickly. In elderly patients, the ability to heal completely and efficiently is critical to making a complete recovery from degenerative conditions, which is what makes umbilical cord-derived stem cells ideal for this age group.
How Stem Cells Change with Age
As we age, our cells (including stem cells) take on different properties. According to a study performed on individuals aged 5 to 80, age was specifically shown to impact the cloning efficiency and proliferation rate of stem cells. In other words, the older cells are, the more limited their cloning potential is. This is important because stem cells’ healing power lies in their ability to proliferate within the joint and create new cartilage.
Umbilical Cells: The Best for Elderly Patients
Researchers note that many of the properties among stem cells derived from adipose and umbilical cord tissues bear strong similarities. Yet, the strong advantages of umbilical cord-derived stem cells, including their ability to outperform other stem cells in terms of proliferation, makes them an attractive option for older adults. More importantly, the critical characteristics of stem cells which change with age are the very factors that make them effective, which is why harvested cells in elderly adults may have limited potential for tissue repair. Thus, while adipose stem cells are highly effective in younger individuals, it is recommended that individuals 65 and older be treated with umbilical cord-derived stem cell sources, as they are more potent in this population for therapeutic applications.





 St. Petersburg, Florida
St. Petersburg, Florida
