Traumatic brain injury (TBI), also known as concussion, is a common condition that affects thousands of people every year in the United States alone. The most challenging aspect of TBI is its vague clinical presentation, which makes it difficult for physicians to promptly diagnose and treat this condition without a proper history of trauma.
According to the Centers for Disease Control and Prevention (CDC), the number of TBI-related hospital visits and deaths increased by 53% between 2006 and 2014. Unfortunately, patients who survive after a concussion often deal with neurological sequela for the rest of their lives. This article will explore the basic concepts of TBI as well as the role of stem cell therapy in restoring normal neurological function after irreversible damage.
How Do Concussions Happen?
The brain is a fragile organ that’s protected by a boney structure known as the skull. Unfortunately, this protection can be a double-edged sword. To prevent contact between the brain and the skull, a liquid called cerebrospinal fluid (CSF) acts as a shock absorber to avoid any trauma to the brain when the skull is abruptly moved. In other words, the brain is floating in the CSF to be able to easily move around when you change positions.
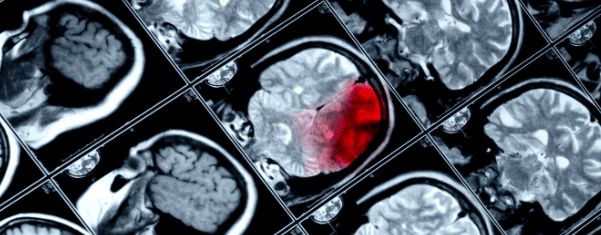
A concussion occurs when the brain collides with the skull at an intensity that surpasses the CSF-cushioning ability. Consequently, the brain will shrink on itself, sending shock waves through the entire tissue, which tear the neurons. This phenomenon is referred to as diffuse axonal injury. As a result, the interneural network responsible for every task that the brain completes is compromised and may lead to irreversible loss of function.
Stem Cell Therapy and Traumatic Brain Injury
Stem cells have the ability to differentiate into several body tissues, which makes them a candidate to treat and repair damage for a myriad of medical conditions, including traumatic brain injuries.
In a clinical trial, researchers used bone marrow-derived stem cells as repair agents to restore the function of damaged brain tissue after enduring TBI. Stem cells were introduced to patients using minimally-invasive procedures with highly-sensitive imaging guidance to deliver the cells at the exact site of tissue damage.
Researchers stated that “These stem cells secrete growth factors that have shown preclinical benefit and also recruit the patient’s own stem cells through various homing signals. Recent successes with similar stem cell therapy trials in other diseases, such as for heart attack recovery, have generated increased interest in now using these approaches to treat brain injury.”
Moreover, a 2018 study published by nature, scientists aimed to find out if certain types of cell therapy, such as umbilical cord stem cells and bone marrow-derived stem cells benefit patients with traumatic brain injuries. The researchers found that these cells can regenerate neurons and repair damage, which may revolutionize the field of traumatology since patients may restore certain neurological functions even after irreversible damage.
Note that the idea of using stem cell therapy to treat concussions is not new, as a 2002 experimental study on rats concluded that “We show for the first time that the IV administration of human umbilical cord blood cells reduces functional deficits after severe traumatic brain injury in the rat. The injected cells enter the brain, migrate into the injured area, and a few express the neuronal and astrocytic phenotypes and integrate into the vascular structures. Cord blood administration may be a useful treatment for traumatic brain injury.”
The use of stem cell therapy to manage symptoms of TBI are still in the experimental phases; however studies have shown its potential to restore lost functions with minimally-invasive procedures that carry an extremely safe side effect profile.
Contact us today!

 St. Petersburg, Florida
St. Petersburg, Florida
