
by admin | Nov 7, 2016 | Studies
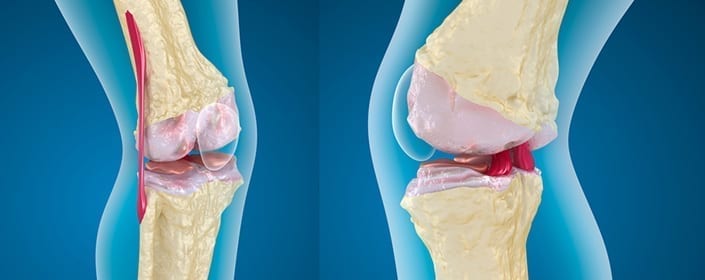
A group of Japanese researchers have just released a study that advances our understanding of how we can use a specific type of stem cells to help patients recover from cartilage damage. This group worked with a specific type of stem cell called bone marrow-derived mesenchymal stem cells (BMSCs) because these cells confer a number of advantages over other types of stem cells that have been used to repair cartilage. Though one particular type of stem cells, called autologous chondrocytes, have been implanted over 20,000 times for therapeutic reasons, these cells are associated with long and arduous surgeries because it is difficult to harvest the required cartilage and periosteum. Another type of stem cell, referred to as suspended cultured chondrocytes, on the other hand, have the potential to result in leakage, with an uneven distribution of cells throughout the site.
Unlike these other stem cell options, BMSCs can be easily harvest through methods that are relatively minimally invasive. The team in Japan also believes that BMSC implantation is safe, as they observed no tumors or infections in the more than 6-year follow-up period of their study. Nonetheless, previous work with BMSC showed that the cells did not lead to the generation of cartilage that was sufficient to replace old cartilage. To overcome that problem, these scientists decided to explore ways to provide large numbers of cells over a short period of time. Because BMSC from humans lose their ability to differentiate into different types of cells after having traveled long distances, the researchers believed that injecting cells directly into the injury site would improve the chances that good cartilage would develop. In addition, adding a specific agent, called, fibroblast growth factor (FGF-2) could help the cells proliferate.
In this study, the researchers tested these ideas to help determine the ideal conditions for transplanting BMSCs for cartilage repair. They found that their method of transplantation led to better cartilage development than was seen in controls, with rats receiving BMSC treated with FGF-2 directly into the area with cartilage injury having higher Wakitani scores. Wakitani scores are used to assess the regeneration of cartilage tissue and how well the new tissue is integrated into the surrounding tissue.
Given that many cartilage defects do not tend to repair themselves and can often lead to osteoarthritis, it is important to find effective ways to regenerate cartilage. There are a number of limitations to the current therapies, but this study demonstrates how our tools for cartilage repair are progressing and the promise of stem cells to help rebuild defective cartilage.
Learn more about using stem cells for orthopedics here.
Reference
Itokazu et al. (2016). Transplantation of scaffold-free cartilage-like cell-sheets made from human bone marrow mesenchymal stem cells for cartilage repair. Cartilage, 7(4), 361-372.

by admin | Oct 20, 2016 | Studies
After following the patients for an average of 2.5 years after their treatment, the scientists concluded that the treatment was safe for this group. No serious adverse side effects were observed in any of the patients.
Researchers in Poland have just published a study aimed at determining whether the use of a particular type of stem cell – known as adipose-derived (from fat tissue) mesenchymal stem cells (ASC’s) is safe for patients. The scientists studied 145 patients, giving them a total of almost 500 injections of ASC’s. After following the patients for an average of 2.5 years after their treatment, the scientists concluded that the treatment was safe for this group and no serious adverse side effects were observed in any of the patients.
Mesenchymal stem cells are regularly transplanted in patients, and hundreds of clinical trials using these cells are underway in the hopes of continuing to identify promising therapeutic options for patients suffering from a wide range of diseases. These cells tend to be collected from either the bone marrow or adipose tissue. Compared to bone marrow, adipose tissue provide the advantage of higher cell numbers, but the safety of using ASC’s from adipose tissue has required confirming the safety and effectiveness of these cells for treatments.
The study undertaken in Poland involved injecting patients with ASC’s as a way to treat orthopedic or neurologic disease. The majority of these patients suffered from injuries involving cartilage, bone, or tendons. The remaining 15 patients had either relapsing-remitting or secondary progressive multiple sclerosis. The only patients that were specifically excluded from the study were those who also suffered from cancer or who were pregnant.
Because safety was the focus of this study, the researchers did not comprehensively study the effect of ASC’s on the patients’ diseases or injuries. Evaluating the long-term effects of ASC transplantation on these patients would require observing the patients over a longer time frame and was outside of the scope of this particular investigation. Nonetheless, the researchers noted that in the time that they monitored these patients, the patients’ clinical symptoms either improved or were not significantly different from the control group, who did not undergo the ASC therapy. No worsening of symptoms was reported.
As more research is done to understand the details of how ASC treatments impact patients, we will gain more information into how safe the treatments are and in what context. Studies continue to show promise for the safety of ASC treatments and the potential to grow this line of therapy into an effective strategy for patients.
Learn more about how adipose stem cells are used to treat brain injury here.
Reference
Siennicka, K. et al. (2016). Adipose-derived cells (stromal vascular fraction) transplanted for orthopedical or neurologcial purposes: are they safe enough? Stem Cells International. http://dx.doi.org/10.1155/2016/5762916

by admin | Jul 25, 2016 | Stem Cell Research, Studies
Research has pointed strongly toward autologous adipose tissue-derived mesencymal stem cells (AdMSC‘s) as a treatment option for a number of neurological diseases. There is growing evidence that these cells can successfully differentiate into neurons in the brain, thereby protecting the brain against certain diseases of the central nervous system. Adipose tissue is particularly attractive when seeking to use mesenchymal stem cells (MSC’s) because it is easy to retrieve MSCs in this type of tissue. Now, a case study published in the Journal of Medical Case Reports demonstrates how AdMSC‘s were successfully used to treat a patient suffering from progressive supranuclear palsy (PSP), a disorder closely related to Parkinson’s disease.
There are currently no good treatment options for PSP. Dopaminergic drugs that are used for Parkinson’s disease are often implemented with PSP patients because of clinical similarities in these diseases. However, the benefits are both minor and short-lived. As described in this case report, researchers successfully used a novel form of therapy on a 71-year old South Korean man with PSP.
The man was examined before his treatment and continually for six months afterwards. The AdMSC protocol improved the patient’s performance on the Progressive Supranuclear Palsy Rating Scale (PSPRS) and improved both his cognitive performance and his ability to conduct daily activities. In addition to the treatment’s efficacy, it also bore limited safety concerns, as mild fever and short-term elevated blood pressure were the only adverse side affects observed with the procedure.
The patient underwent four intrathecal and five intravenous infusions infusions of AdMSC’s to increase the chances of clinical efficacy. Specifically, the strategy of the intrathecal infusions was to increase the likelihood of getting the AdMSC’s into the central nervous system. However, because the intrathecal cavity is narrow, the dosage that can be achieved through this route is limited. Thus, intravenous injections were administered as a way to increase the dosage amount. Though this success of AdMSC’s administration in PSP is just the beginning, it represents great potential for the use of stem cells in this rare but deadly disorder.
To learn more about the safety of adipose stem cell procedure, click here.
Reference
Choi, S.W., Park, K.B., Woo, S.K., Kang, S.K., & Ra, J.C. (2014). Treatment of progressive supranuclear palsy with autologous adipose tissue-derived mesenchymal stem cells: a case report. Journal of Medical Case Reports, 8(87), 1-5.

by admin | May 9, 2016 | Studies
Both Hyperbaric Oxygen (HBO) treatment and Mesenchymal Stem Cells (MSC‘s) have been used as interventions for patients suffering from Traumatic Brain Injury (TBI). Though each of these therapeutic approaches can confer benefits to patients, researchers have shown that combining the two techniques can yield better results for this population of patients than either method can achieve alone. The scientists published their findings in Neural Regeneration Research earlier this year.
The transplantation of MSC‘s and the use of HBO are each effective in treating TBI for different reasons. Mesenchymal stem cells can proliferate rapidly, differentiate into many different types of cells, and do not tend to cause adverse immune reactions. While HBO treatment can enhance the brain’s aerobic metabolism, providing brain tissue with more oxygen. All of these effects are helpful after TBI has occurred. However, MSC‘s alone can be limiting in their therapeutic potential because only a fraction of those that are transplanted differentiate into mature brain cells. Because hyperbaric oxygen treatment both protects injured tissue and also supports the differentiation and migration of MSC‘s, researchers hypothesized that combining the therapies would improve lead to better neurological and cognitive outcomes following TBI than either treatment would alone.
To test their idea, the scientists induced TBI in rats to establish a rat model of the condition. They then treated one group of rats with just HBO, transplanted MSC‘s in another group of rats that did not undergo HBO, and used both interventions in a final group of rats. The researchers then looked both at physiological markers associated with TBI, as well as cognitive performance on a learning and memory task.
The results showed that rats that underwent both MSC‘s transplantation and HBO had better neurological outcomes and better cognitive performance scores than rats that endured only one type of treatment. Given these promising findings in an animal model of TBI, future research will likely address the translatability of these findings to humans. Now that a proof-of-concept exercise has been successful, there is significant support for the potential of this combination treatment regimen to help people who experience TBI.
Reference
Zhou, H. X., Liu, Z. G., Liu, X. J., & Chen, Q. X. (2016). Umbilical cord-derived mesenchymal stem cell transplantation combined with hyperbaric oxygen treatment for repair of traumatic brain injury. Neural Regen Res, 11(1), 107-113. doi: 10.4103/1673-5374.175054

by admin | Mar 21, 2016 | Parkinson's Disease, Studies
Though research has shown that stem cells are therapeutic candidates for neurodegenerative diseases like Parkinson’s disease, scientists have been working on overcoming the challenges associated with effectively delivering these cells to the brain. A recent study, published in the journal Rejuvenation Research, demonstrated that intranasal delivery of stem cells provided both physiological and behavioral benefits in a rat model of Parkinson’s disease.
Once researchers had determined that stem cells could help patients suffering from brain disorders, a number of interventions were attempted. Surgical transplantation, though invasive, has been a popular method for direct stem cell delivery to the brain. However, this technique often causes local trauma and also tends to leads to problematic immune responses that make the transplant ineffective. Delivering cells through veins or arteries is a less invasive method for providing the brain with these cells, but this method can be less effective, with the cells sometimes traveling to organs other than the brain and becoming trapped there.
In their article, Therapeutic Efficacy of Intranasally Delivered Mesenchymal Stem Cells in a Rat Model of Parkinson Disease, Lusine Danielyan and colleagues describe their previous work that showed that intranasal application of mesenchymal stem cells lead to the successful integration of these cells in parts of the brain that are critical in Parkinson’s disease. Building on this work, they now show that intransal delivery of stem cells is not only feasible but has practical clinical applications. In a rat model of Parkinson’s disease, rats normally experience dopamine depletion in certain areas of the barin, as well as increased levels of inflammatory cytokines, which are cells of the immune system. Intransal administration of stem cells prevented both of these effects in the rat model.
Of particular significance is that researchers did more than show that intranasal delivery of stem cells leads to physiological changes that are consistent with effective Parkinson’s disease therapy. They also showed that the technique had therapeutic behavioral effects. When intranasal administration of stem cells was applied to the rat model of Parkinson’s dieases, motor function improved. As motor dysfunction is a hallmark of Parkinson’s disease, this finding demonstrates the significant promise that intransal delivery of stem cells holds for treating Parkinson’s disease.
Reference
Danielyan, L., Schafer, R., von Ameln-Mayerhofer, A., Bernhard, F., Verleysdonk, S., Buadze, M., . . . Frey, W. H., 2nd. (2011). Therapeutic efficacy of intranasally delivered mesenchymal stem cells in a rat model of Parkinson disease. Rejuvenation Res, 14(1), 3-16. doi: 10.1089/rej.2010.1130





 St. Petersburg, Florida
St. Petersburg, Florida
